Bled to death
-
I get a medical malpractice newsletter. Some of it covers pretty routine stuff.
I found this one shocking.
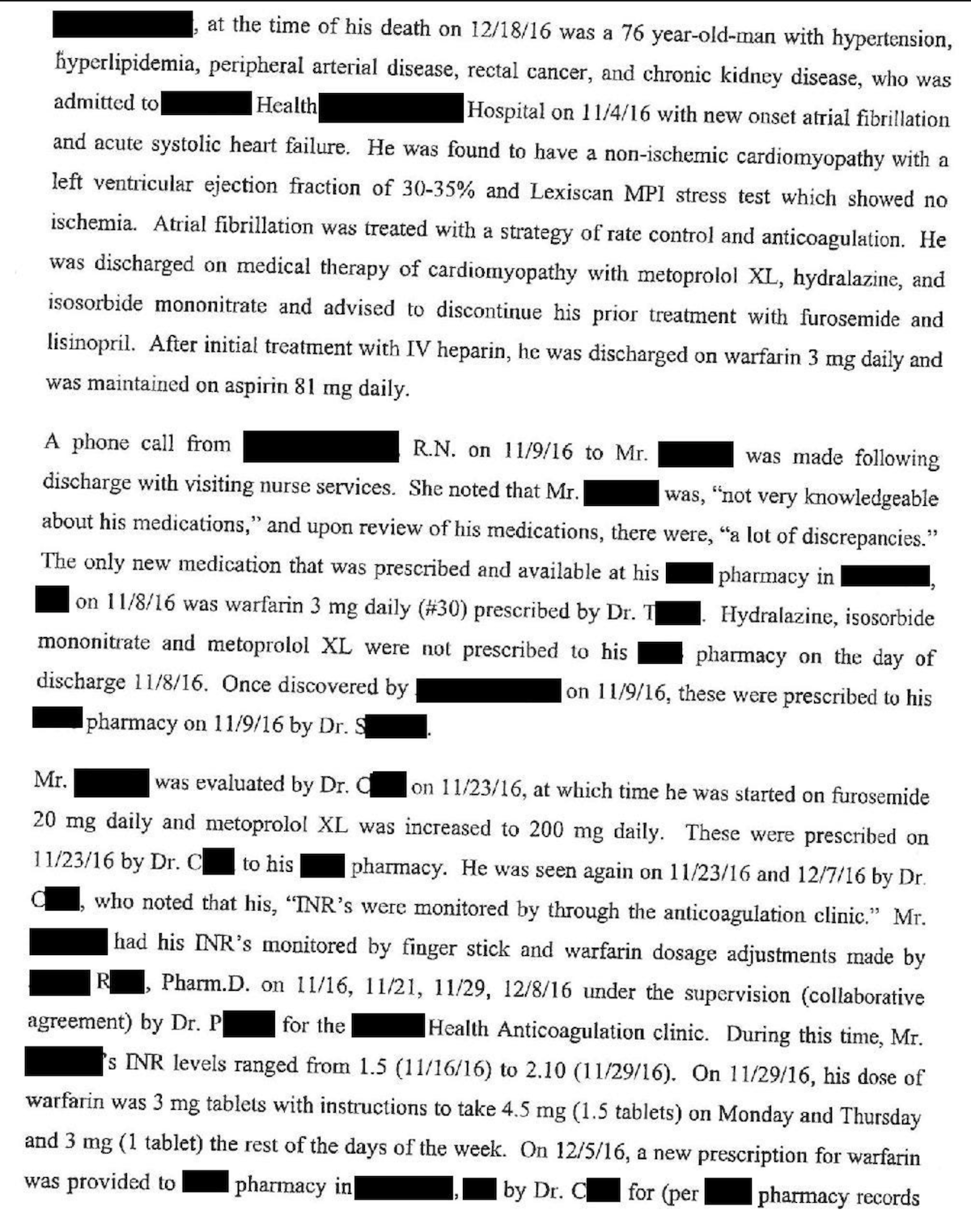
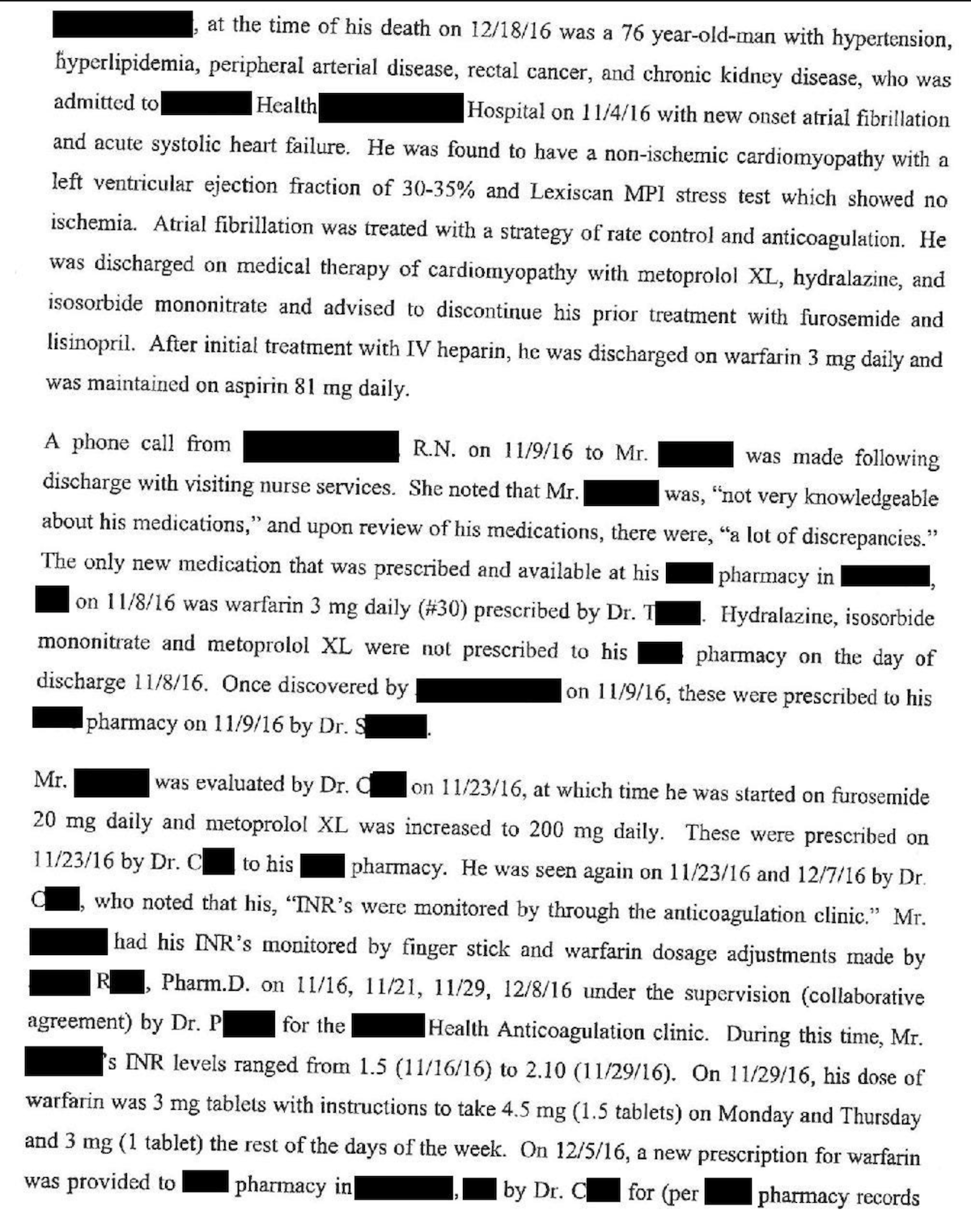
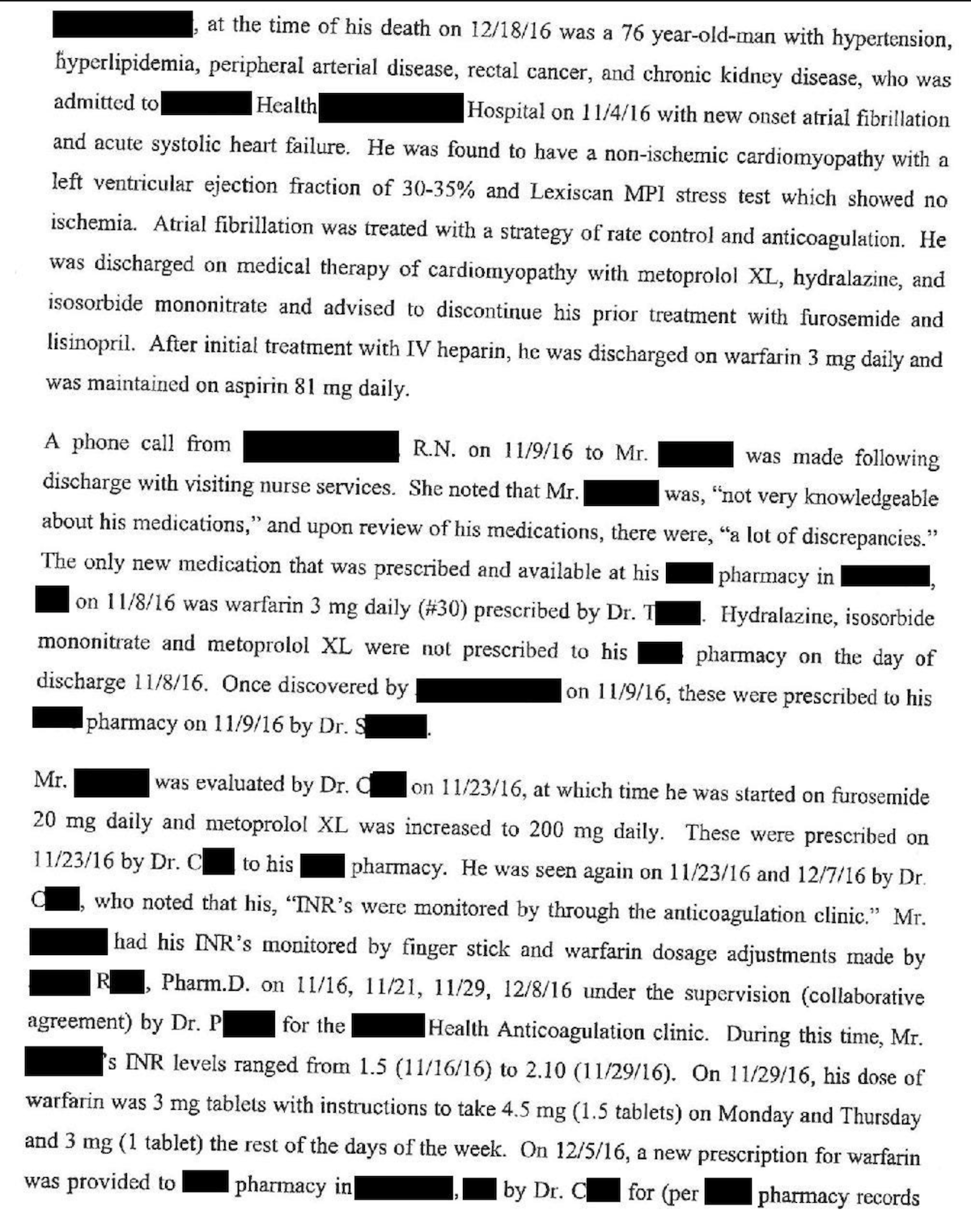
Patient gets admitted with a new onset of atrial fibrillation to the emergency room. His a fib converts to regular rhythm, and he has started on a blood thinner, warfarin, also known as Coumadin. He is told to take the warfarin 3 mg a day, and his anticoagulation status will be reviewed.
After taking the Coumadin, his coagulation is still not up to where it should be. He was being managed in the coagulation clinic.
Three weeks later, his coagulation was still not quite controlled and he was instructed to take one and a half tablets ( 4.5 mg) parenthesis two days a week and 13 mg tablet on the other days of the week.
He was running out of warfarin, so he called his cardiologist office for a refill, and the nurse called in a refill for him. The message indicated that he should take “4.5” on 2 days per week, and “3” on the remaining days.
Unfortunately, the message was left without specifying the units of these doses. The nurse meant 3 milligrams per day, but the pharmacist filled it as 3 tablets per day.
On the other days of the week, the prescription indicated he should take 4.5 tablets per day (as opposed to the correct dose of 4.5mg).
The patient noticed, increased, bleeding, and bruising. His anticoagulation was sky high.
Long story short, he was found in a pool of blood, and died the next day in the hospital.
-
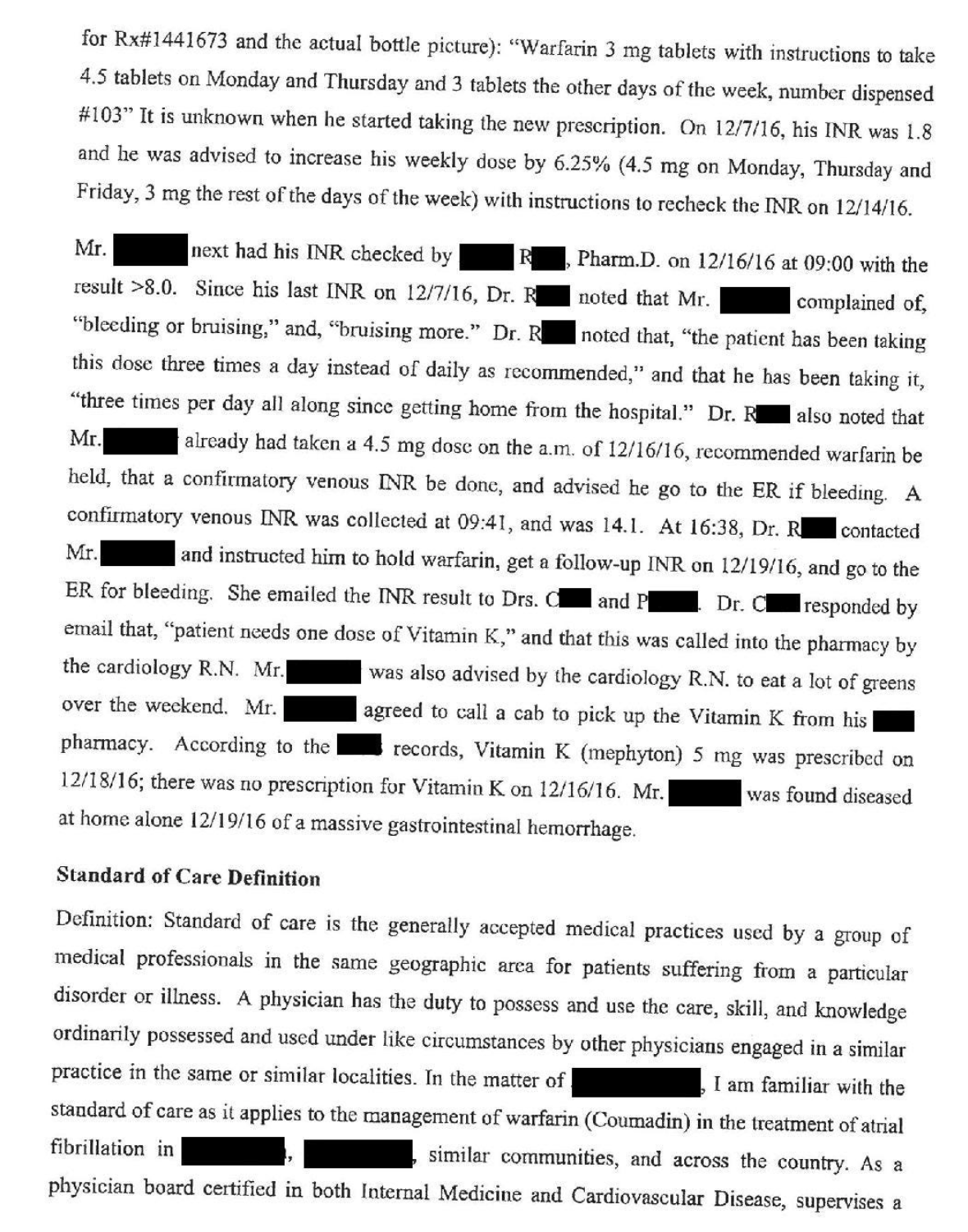
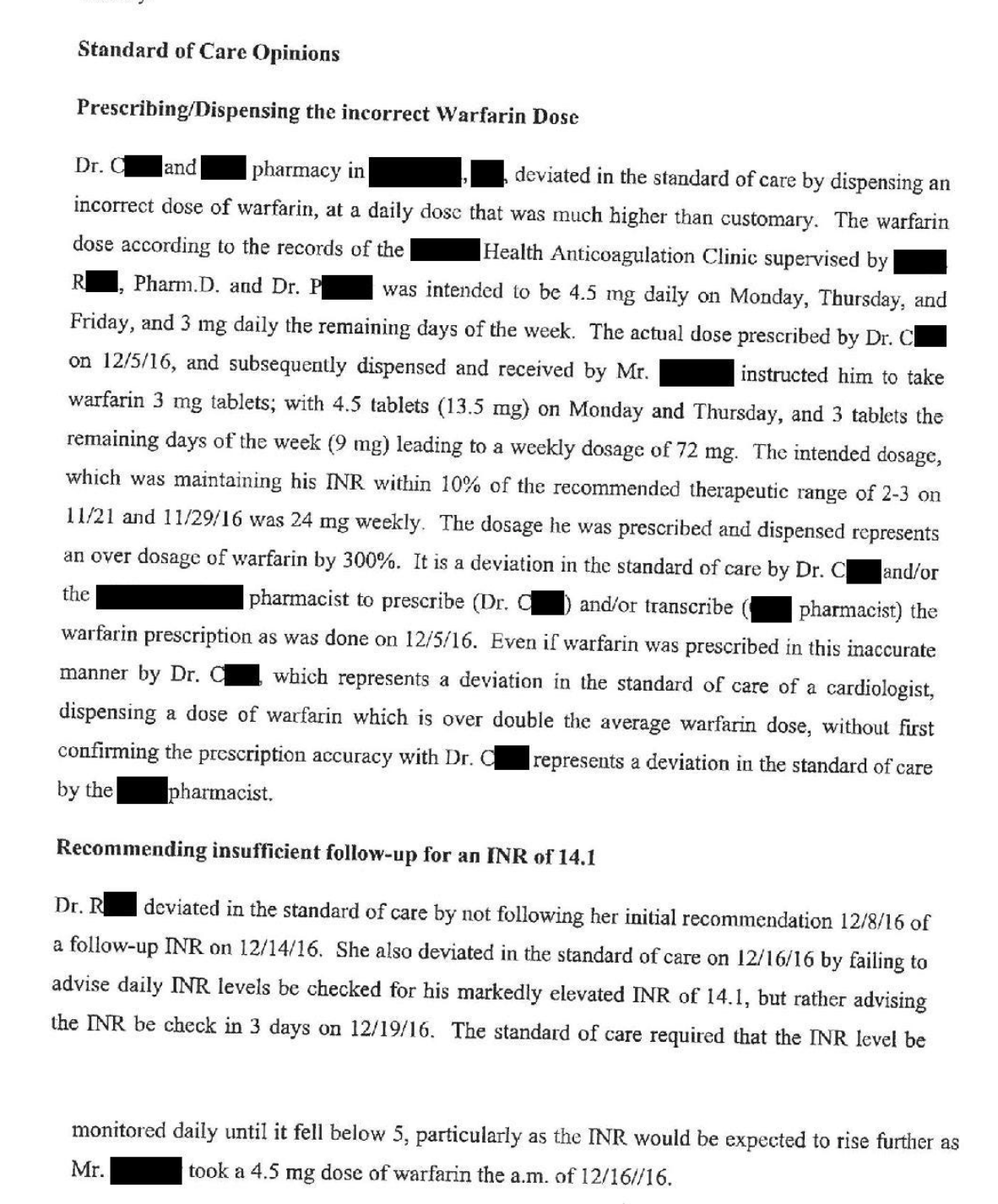
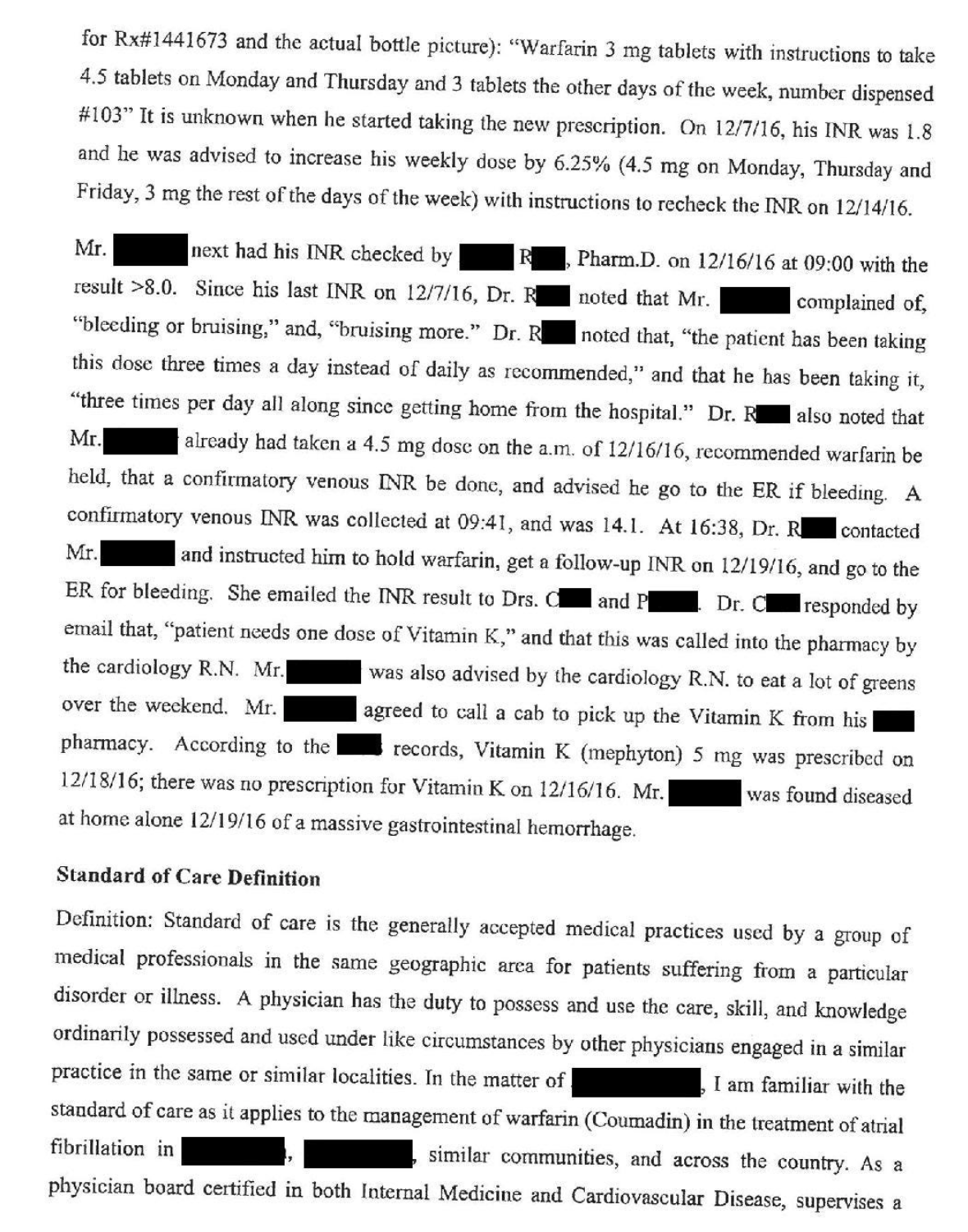
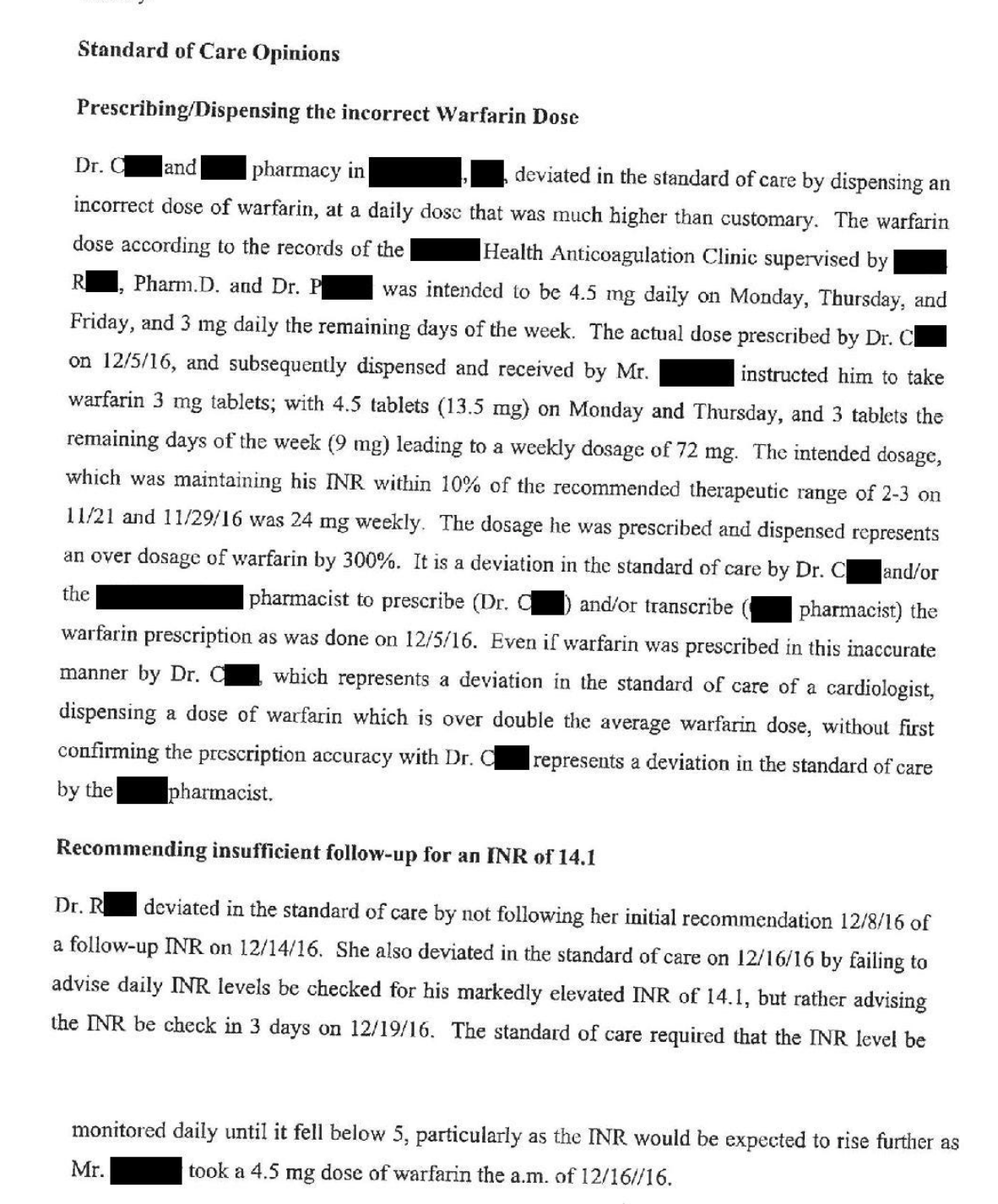
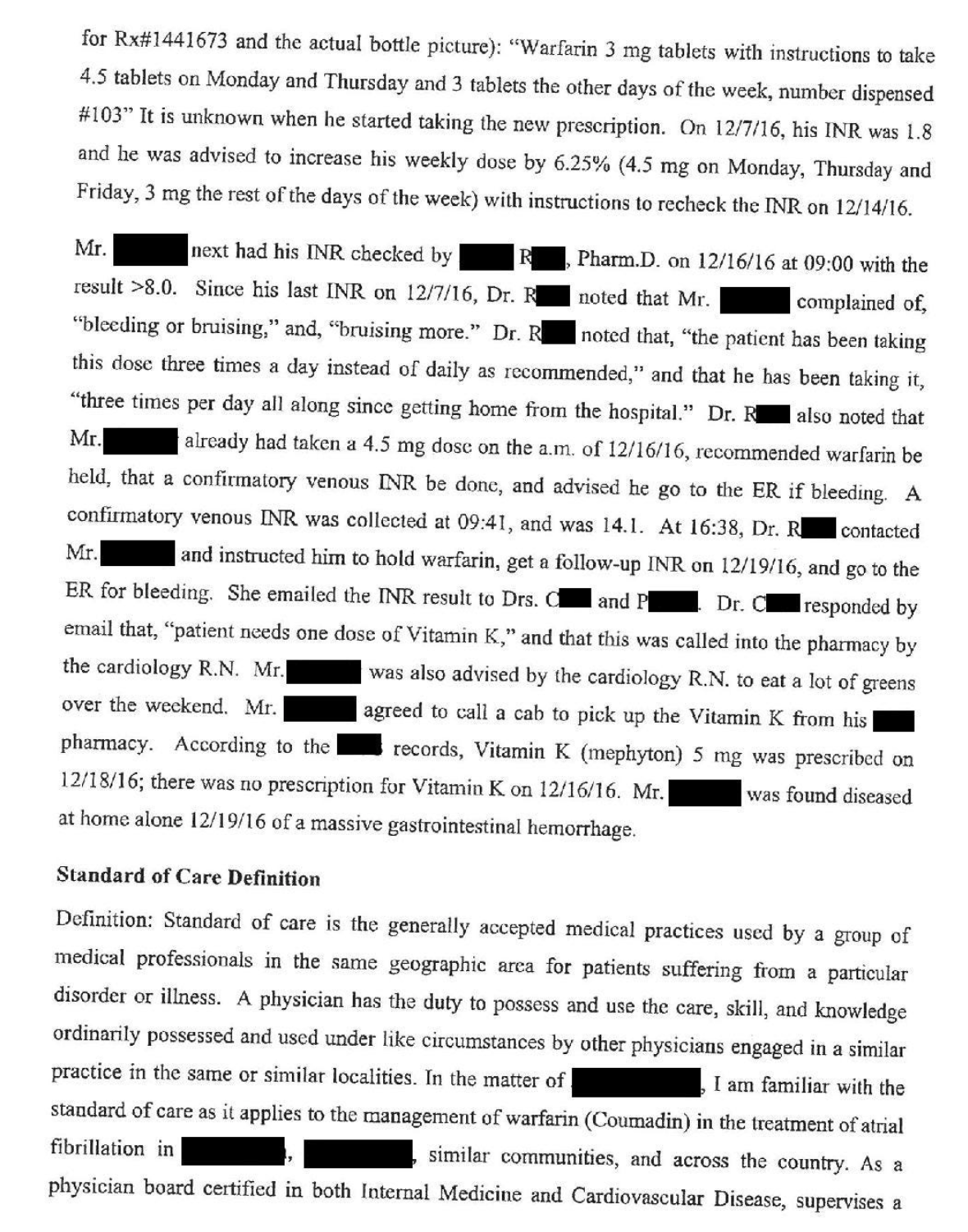
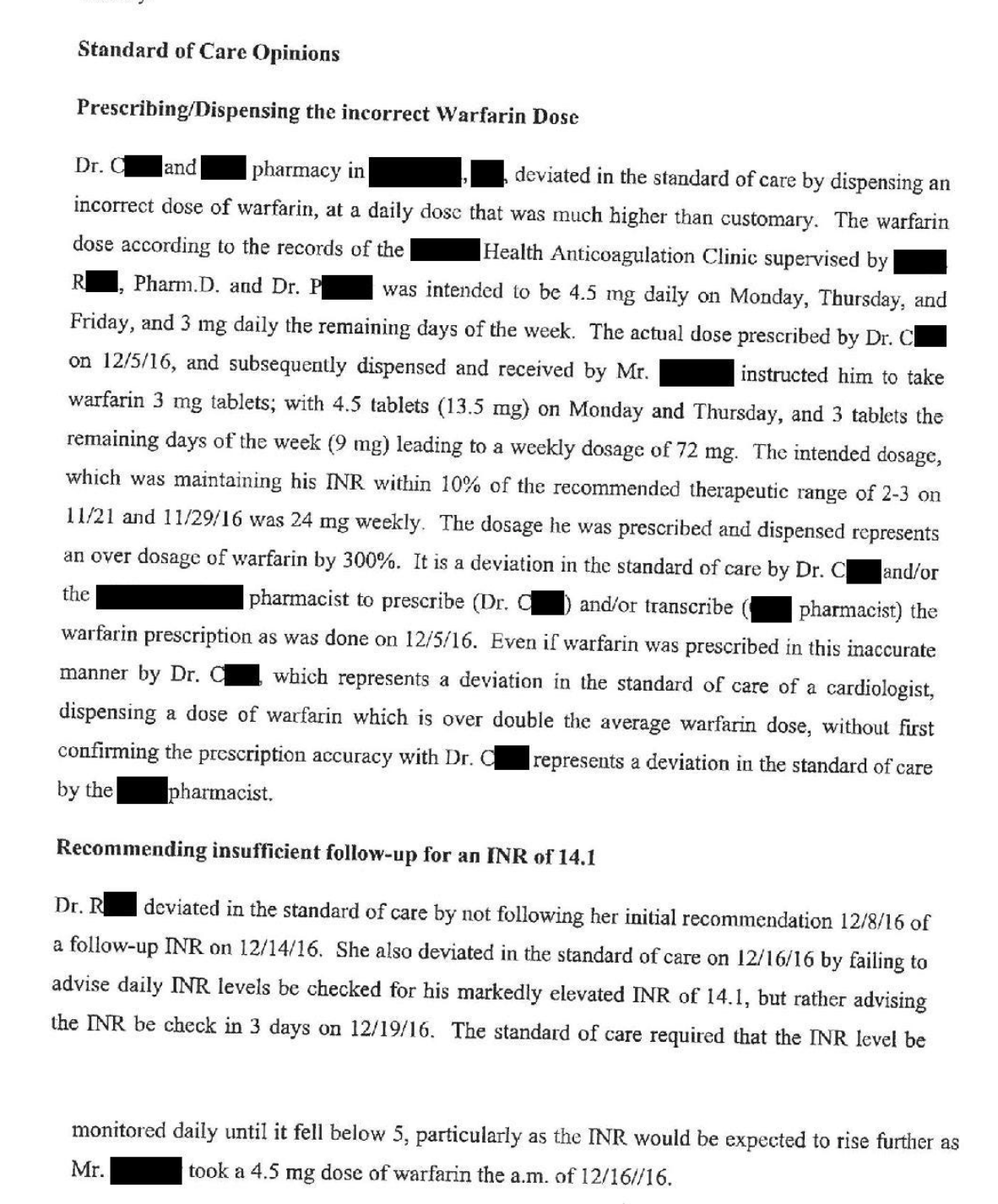
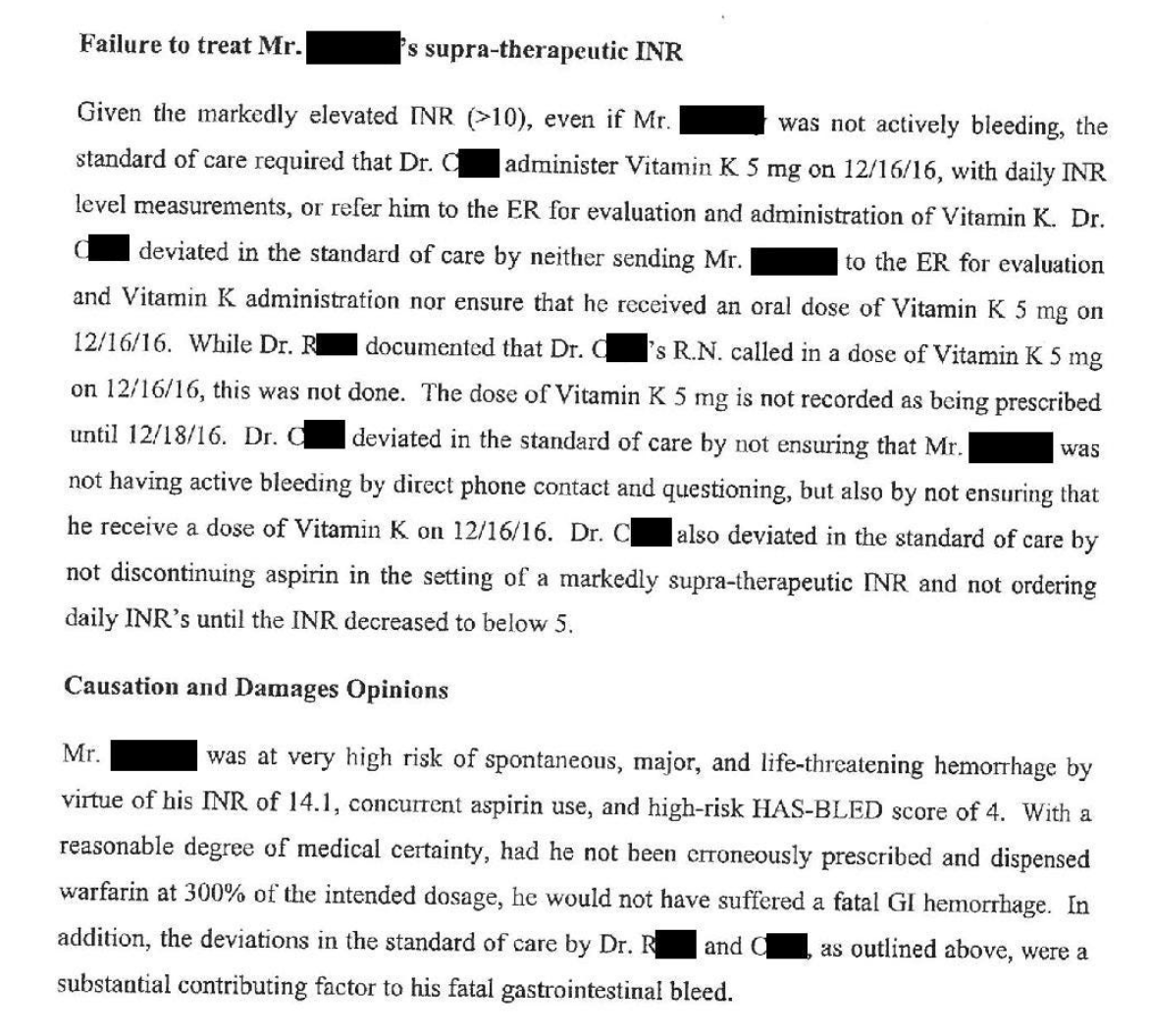
THe docs in this case were dropped from the lawsuit.
Only the hospital (and presumable the RN who was unclear in the order) settled for $750K.
If you’re interested in the expret witness testimony:
The newsletter comments:
- This case is fundamentally about a failure to communicate. The nurse and the pharmacist both felt that the instructions were clear, and didn’t realize the mistake until it was too late. Providing a written or electronic prescription would have reduced the likelihood of this error.
- While I was reflecting on this case, I remembered the words of some of my math and science teachers from as far back as grade school, admonishing students to label their units. It can be frustrating for students to miss points because they had the correct number but didn’t appropriately label the units, but this case is a perfect example of why its important.
- Medications with complicated dosing regimens are inherently more dangerous. This is readily apparent when comparing warfarin and factor Xa inhibitors. This case happened in 2016, long after the factor Xa inhibitors were available. I wonder if the higher price of the factor Xa inhibitors is what prompted them to choose warfarin.
- The communication between the coagulation clinic and Dr. C’s office made this situation much worse. It appears that the coagulation clinic was responsible for monitoring his INR and suggesting changes, but they did not actually manage the warfarin prescription. The prescriptions were routed through Dr. C’s office, creating a game of telephone that introduced both errors and significant delays.
Considering his INR was so high - I wonder if they’d considered FFP to get it down. Vitamin K takes a long time.
-
I get a medical malpractice newsletter. Some of it covers pretty routine stuff.
I found this one shocking.
Patient gets admitted with a new onset of atrial fibrillation to the emergency room. His a fib converts to regular rhythm, and he has started on a blood thinner, warfarin, also known as Coumadin. He is told to take the warfarin 3 mg a day, and his anticoagulation status will be reviewed.
After taking the Coumadin, his coagulation is still not up to where it should be. He was being managed in the coagulation clinic.
Three weeks later, his coagulation was still not quite controlled and he was instructed to take one and a half tablets ( 4.5 mg) parenthesis two days a week and 13 mg tablet on the other days of the week.
He was running out of warfarin, so he called his cardiologist office for a refill, and the nurse called in a refill for him. The message indicated that he should take “4.5” on 2 days per week, and “3” on the remaining days.
Unfortunately, the message was left without specifying the units of these doses. The nurse meant 3 milligrams per day, but the pharmacist filled it as 3 tablets per day.
On the other days of the week, the prescription indicated he should take 4.5 tablets per day (as opposed to the correct dose of 4.5mg).
The patient noticed, increased, bleeding, and bruising. His anticoagulation was sky high.
Long story short, he was found in a pool of blood, and died the next day in the hospital.
@George-K said in Bled to death:
After taking the Coumadin, his coagulation is still not up to where it should be.
Kind of a technical question:
Coagulation is the clotting of blood. If his blood was not clotting, why would he be taking a blood thinner? That would seem to make it worse. What am I missing?
-
THe docs in this case were dropped from the lawsuit.
Only the hospital (and presumable the RN who was unclear in the order) settled for $750K.
If you’re interested in the expret witness testimony:
The newsletter comments:
- This case is fundamentally about a failure to communicate. The nurse and the pharmacist both felt that the instructions were clear, and didn’t realize the mistake until it was too late. Providing a written or electronic prescription would have reduced the likelihood of this error.
- While I was reflecting on this case, I remembered the words of some of my math and science teachers from as far back as grade school, admonishing students to label their units. It can be frustrating for students to miss points because they had the correct number but didn’t appropriately label the units, but this case is a perfect example of why its important.
- Medications with complicated dosing regimens are inherently more dangerous. This is readily apparent when comparing warfarin and factor Xa inhibitors. This case happened in 2016, long after the factor Xa inhibitors were available. I wonder if the higher price of the factor Xa inhibitors is what prompted them to choose warfarin.
- The communication between the coagulation clinic and Dr. C’s office made this situation much worse. It appears that the coagulation clinic was responsible for monitoring his INR and suggesting changes, but they did not actually manage the warfarin prescription. The prescriptions were routed through Dr. C’s office, creating a game of telephone that introduced both errors and significant delays.
Considering his INR was so high - I wonder if they’d considered FFP to get it down. Vitamin K takes a long time.
@George-K said in Bled to death:
THe docs in this case were dropped from the lawsuit.
Only the hospital (and presumable the RN who was unclear in the order) settled for $750K.
If you’re interested in the expret witness testimony:
The newsletter comments:
- This case is fundamentally about a failure to communicate. The nurse and the pharmacist both felt that the instructions were clear, and didn’t realize the mistake until it was too late. Providing a written or electronic prescription would have reduced the likelihood of this error.
- While I was reflecting on this case, I remembered the words of some of my math and science teachers from as far back as grade school, admonishing students to label their units. It can be frustrating for students to miss points because they had the correct number but didn’t appropriately label the units, but this case is a perfect example of why its important.
- Medications with complicated dosing regimens are inherently more dangerous. This is readily apparent when comparing warfarin and factor Xa inhibitors. This case happened in 2016, long after the factor Xa inhibitors were available. I wonder if the higher price of the factor Xa inhibitors is what prompted them to choose warfarin.
- The communication between the coagulation clinic and Dr. C’s office made this situation much worse. It appears that the coagulation clinic was responsible for monitoring his INR and suggesting changes, but they did not actually manage the warfarin prescription. The prescriptions were routed through Dr. C’s office, creating a game of telephone that introduced both errors and significant delays.
Considering his INR was so high - I wonder if they’d considered FFP to get it down. Vitamin K takes a long time.
FFP + Cryo.
-
@George-K said in Bled to death:
After taking the Coumadin, his coagulation is still not up to where it should be.
Kind of a technical question:
Coagulation is the clotting of blood. If his blood was not clotting, why would he be taking a blood thinner? That would seem to make it worse. What am I missing?
@taiwan_girl said in Bled to death:
Coagulation is the clotting of blood. If his blood was not clotting, why would he be taking a blood thinner? That would seem to make it worse. What am I missing?
"Blood thinner" is a colloquialism for an anticoagulant.
Warfarin was the anticoagulant - the "thinner."