More masks....
-
This journal is highly respected, right up there with NEJM
https://www.acpjournals.org/doi/10.7326/M20-6817
Results:
A total of 3030 participants were randomly assigned to the recommendation to wear masks, and 2994 were assigned to control; 4862 completed the study. Infection with SARS-CoV-2 occurred in 42 participants recommended masks (1.8%) and 53 control participants (2.1%). The between-group difference was −0.3 percentage point (95% CI, −1.2 to 0.4 percentage point; P = 0.38) (odds ratio, 0.82 [CI, 0.54 to 1.23]; P = 0.33). Multiple imputation accounting for loss to follow-up yielded similar results. Although the difference observed was not statistically significant, the 95% CIs are compatible with a 46% reduction to a 23% increase in infection.
Conclusion:
The recommendation to wear surgical masks to supplement other public health measures did not reduce the SARS-CoV-2 infection rate among wearers by more than 50% in a community with modest infection rates, some degree of social distancing, and uncommon general mask use. The data were compatible with lesser degrees of self-protection.
The long discussion:
n this community-based, randomized controlled trial conducted in a setting where mask wearing was uncommon and was not among other recommended public health measures related to COVID-19, a recommendation to wear a surgical mask when outside the home among others did not reduce, at conventional levels of statistical significance, incident SARS-CoV-2 infection compared with no mask recommendation. We designed the study to detect a reduction in infection rate from 2% to 1%. Although no statistically significant difference in SARS-CoV-2 incidence was observed, the 95% CIs are compatible with a possible 46% reduction to 23% increase in infection among mask wearers. These findings do offer evidence about the degree of protection mask wearers can anticipate in a setting where others are not wearing masks and where other public health measures, including social distancing, are in effect. The findings, however, should not be used to conclude that a recommendation for everyone to wear masks in the community would not be effective in reducing SARS-CoV-2 infections, because the trial did not test the role of masks in source control of SARS-CoV-2 infection. During the study period, authorities did not recommend face mask use outside hospital settings and mask use was rare in community settings (22). This means that study participants' exposure was overwhelmingly to persons not wearing masks.
The observed infection rate was similar to that reported in other large Danish studies during the study period (26, 30). Of note, the observed incidence of SARS-CoV-2 infection was higher than we had estimated when planning a sample size that would ensure more than 80% power to detect a 50% decrease in infection. The intervention lasted only 1 month and was carried out during a period when Danish authorities recommended quarantine of diagnosed patients, physical distancing, and hand hygiene as general protective means against SARS-CoV-2 transmission (23). Cafés and restaurants were closed through 18 May, but follow-up of the second randomized group continued through 2 June.
The first randomized group was followed while the Danish society was under lockdown. Reopening occurred (18 May 2020) during follow-up of the second group of participants, but it was not reflected in the outcome because infection rates were similar between groups (Supplement Figure 2). The relative infection rate between mask wearers and those not wearing masks would most likely be affected by changes in applied protective means or in the virulence of SARS-CoV-2, whereas the rate difference between the 2 groups would probably not be affected solely by a higher—or lower—number of infected citizens.
Although we saw no statistically significant difference in presence of other respiratory viruses, the study was not sufficiently powered to draw definite conclusions about the protective effect of masks for other viral infections. Likewise, the study had limited power for any of the subgroup analyses.
The primary outcome was mainly defined by antibodies against SARS-CoV-2. This definition was chosen because the viral load of infected patients may be only transiently detectable (31, 32) and because approximately half of persons infected with SARS-CoV-2 are asymptomatic (33, 26). Masks have been hypothesized to reduce inoculum size (34) and could increase the likelihood that infected mask users are asymptomatic, but this hypothesis has been challenged (35). For these reasons, we did not rely solely on identification of SARS-CoV-2 in oropharyngeal/nasal swab samples. As mentioned in the Methods section, an internal validation study estimated that the point-of-care test has 82.5% sensitivity and 99.5% specificity (26).
The observed rate of incident SARS-CoV-2 infection was similar to what was estimated during trial design. These rates were based on thorough screening of all participants using antibody measurements combined with PCR, whereas the observed official infection rates relied solely on PCR test–based estimates during the period. In addition, authorities tested only a small subset of primarily symptomatic citizens of the entire population, yielding low incidence rates. On this basis, the infection rates we report here are not comparable with the official SARS-CoV-2 infection rates in the Danish population. The eligibility requirement of at least 3 hours of exposure to other persons outside the home would add to this difference. Between 6 April and 9 May 2020, we found a similar seroprevalence of SARS-CoV-2 of 1.9% (CI, 0.8% to 2.3%) in Danish blood donors using the Livzon point-of-care test and assessed by laboratory technicians (36). Testing at the end of follow-up, however, may not have captured any infections contracted during the last part of the study period, but this would have been true in both the mask and control groups and was not expected to influence the overall findings.
The face masks provided to participants were high-quality surgical masks with a filtration rate of 98% (37). A published meta-analysis found no statistically significant difference in preventing influenza in health care workers between respirators (N95 [American standard] or FFP2 [European standard]) and surgical face masks (38). Adherence to mask use may be higher than observed in this study in settings where mask use is common. Some mask group participants (14%) reported adverse reactions from other citizens (Supplement Table 4). Although adherence may influence the protective effect of masks, sensitivity analyses had similar results across reported adherence.
How SARS-CoV-2 is transmitted—via respiratory droplets, aerosols, or (to a lesser extent) fomites—is not firmly established. Droplets are larger and rapidly fall to the ground, whereas aerosols are smaller (≤5 μm) and may evaporate and remain in the air for hours (39). Transmission of SARS-CoV-2 may take place through multiple routes. It has been argued that for the primary route of SARS-CoV-2 spread—that is, via droplets—face masks would be considered effective, whereas masks would not be effective against spread via aerosols, which might penetrate or circumnavigate a face mask (37, 39). Thus, spread of SARS-CoV-2 via aerosols would at least partially explain the present findings. Lack of eye protection may also have been of importance, and use of face shields also covering the eyes (rather than face masks only) has been advocated to halt the conjunctival route of transmission (40, 41). We observed no statistically significant interaction between wearers and nonwearers of eyeglasses (Supplement Figure 2). Recent reports indicate that transmission of SARS-CoV-2 via fomites is unusual (42), but masks may alter behavior and potentially affect fomite transmission.
The present findings are compatible with the findings of a review of randomized controlled trials of the efficacy of face masks for prevention (as personal protective equipment) against influenza virus (18). A recent meta-analysis that suggested a protective effect of face masks in the non–health care setting was based on 3 observational studies that included a total of 725 participants and focused on transmission of SARS-CoV-1 rather than SARS-CoV-2 (12). Of 725 participants, 138 (19%) were infected, so the transmission rate seems to be higher than for SARS-CoV-2. Further, these studies focused on prevention of infection in healthy mask wearers from patients with a known, diagnosed infection rather than prevention of transmission from persons in their surroundings in general. In addition, identified comparators (control participants) not wearing masks may also have missed other protective means. Recent observational studies that indicate a protective association between mandated mask use in the community and SARS-CoV-2 transmission are limited by study design and simultaneous introduction of other public health interventions (14, 43).
Several challenges regarding wearing disposable face masks in the community exist. These include practical aspects, such as potential incorrect wearing, reduced adherence, reduced durability of the mask depending on type of mask and occupation, and weather. Such circumstances may necessitate the use of multiple face masks during the day. In our study, participants used a mean of 1.7 masks per weekday and 1.3 per weekend day (Supplement Table 4). Wearing a face mask may be physically unpleasant, and psychological barriers and other side effects have been described (44). “Face mask policing” between citizens might reinforce use of masks but may be challenging. In addition, the wearer of a face mask may change to a less cautious behavior because of a false sense of security, as pointed out by WHO (17); accordingly, our face mask group seemed less worried (Supplement Table 4), which may explain their increased willingness to wear face masks in the future (Supplement Table 5). These challenges, including costs and availability, may reduce the efficacy of face masks to prevent SARS-CoV-2 infection.
The potential benefits of a community-wide recommendation to wear masks include combined prevention and source control for symptomatic and asymptomatic persons, improved attention, and reduced potential stigmatization of persons wearing masks to prevent infection of others (17). Although masks may also have served as source control in SARS-CoV-2–infected participants, the study was not designed to determine the effectiveness of source control.
The most important limitation is that the findings are inconclusive, with CIs compatible with a 46% decrease to a 23% increase in infection. Other limitations include the following. Participants may have been more cautious and focused on hygiene than the general population; however, the observed infection rate was similar to findings of other studies in Denmark (26, 30). Loss to follow-up was 19%, but results of multiple imputation accounting for missing data were similar to the main results. In addition, we relied on patient-reported findings on home antibody tests, and blinding to the intervention was not possible. Finally, a randomized controlled trial provides high-level evidence for treatment effects but can be prone to reduced external validity.
Our results suggest that the recommendation to wear a surgical mask when outside the home among others did not reduce, at conventional levels of statistical significance, the incidence of SARS-CoV-2 infection in mask wearers in a setting where social distancing and other public health measures were in effect, mask recommendations were not among those measures, and community use of masks was uncommon. Yet, the findings were inconclusive and cannot definitively exclude a 46% reduction to a 23% increase in infection of mask wearers in such a setting. It is important to emphasize that this trial did not address the effects of masks as source control or as protection in settings where social distancing and other public health measures are not in effect.
Reduction in release of virus from infected persons into the environment may be the mechanism for mitigation of transmission in communities where mask use is common or mandated, as noted in observational studies. Thus, these findings do not provide data on the effectiveness of widespread mask wearing in the community in reducing SARS-CoV-2 infections. They do, however, offer evidence about the degree of protection mask wearers can anticipate in a setting where others are not wearing masks and where other public health measures, including social distancing, are in effect. The findings also suggest that persons should not abandon other COVID-19 safety measures regardless of the use of masks. While we await additional data to inform mask recommendations, communities must balance the seriousness of COVID-19, uncertainty about the degree of source control and protective effect, and the absence of data suggesting serious adverse effects of masks (45).
-
"Did not reduce by more than 50%" is rather odd wording. Why didn't they
say 'reduced by between 23% and 46%' which I think is what they ended up saying?IOW, masks probably reduce infection, but there's a shit ton of other factors and it's actually really hard to measure and bloody complicated.
-
"Did not reduce by more than 50%" is rather odd wording. Why didn't they
say 'reduced by between 23% and 46%' which I think is what they ended up saying?IOW, masks probably reduce infection, but there's a shit ton of other factors and it's actually really hard to measure and bloody complicated.
@Doctor-Phibes said in More masks....:
bloody complicated.
That, basically, is my take.
We just don't know, and I'll err on the side of caution.
-
This is really talking about being the guy with the mask in a community where mask usage is uncommon.
The real gains come from community usage. There’s truth behind those silly memes.
@jon-nyc said in More masks....:
This is really talking about being the guy with the mask in a community where mask usage is uncommon.
No, they specifically pointed out that mask usage in this community is unusually high.
My take? Masks help a little. Not nearly as much as Social Distancing and hand washing, but some small amount. Plus, masks are easier to mandate and enforce than social distancing and handwashing.
The problem is that way too many are looking at masks as the Great White Hope. They aren’t. They make some slight difference, but are possibly doing more harm than good because people aren’t social distancing and washing because they think the masks are protecting them...
There’s a reason why this shit’s spiking in areas with mask mandates just as much as those that don’t... 85% of those testing positive are mask wearers....
-
I think it also depends on the type of mask. We've gone to DEFCON 2 which for me means a double mask - a surgiclal mask plus N95 mask over it when entering a store. I also wear latex gloves when entering the store which are removed immediately after leaving. Hands are washed upon entering the house. We have as much delivered as possible but still need to visit the store a couple of times a week.
I see a lot of people wearing masks as chin guards - and some masks are just cloth which is really imaginary protection.
I run in the forest preserve and wear a cloth covering there - which I understand is imaginary but I also stay 10 or more feet away from people and the 30 mph wind helps to ensure minimal exposure.
-
My wife makes me wear a mask in bed. For some reason it's got this Patrick Dempsey face stenciled on it. Better safe than sorry, I guess, and he's a doctor and everything.
-
Hi - been a long time, since I've checked this forum.
I didn't read the entire article, but what is irritating is when employees of stores we shop at, as well as customers, wear a bandana, that they loosely just tie on, or a gaiter. Neither a bandana or gaiter help as well as a regular "single use" mask. I understand that grocery stores and other sites are pushing sales of gaiters, which people rarely wore in the past!
We are in the PURPLE here in California. -
"Did not reduce by more than 50%" is rather odd wording. Why didn't they
say 'reduced by between 23% and 46%' which I think is what they ended up saying?IOW, masks probably reduce infection, but there's a shit ton of other factors and it's actually really hard to measure and bloody complicated.
@Doctor-Phibes said in More masks....:
"Did not reduce by more than 50%" is rather odd wording. Why didn't they
say 'reduced by between 23% and 46%' which I think is what they ended up saying?IOW, masks probably reduce infection, but there's a shit ton of other factors and it's actually really hard to measure and bloody complicated.
Yes, the words are confusing.
They said
Yet, the findings were inconclusive and cannot definitively exclude a 46% reduction to a 23% increase in infection of mask wearers in such a setting.
I think that actually means, wearing masks has a range of effects from:
a 46% reduction in infections to
a 23% increase in infectionsI think it says a mask can increase infections
-
@jon-nyc said in More masks....:
This is really talking about being the guy with the mask in a community where mask usage is uncommon.
No, they specifically pointed out that mask usage in this community is unusually high.
My take? Masks help a little. Not nearly as much as Social Distancing and hand washing, but some small amount. Plus, masks are easier to mandate and enforce than social distancing and handwashing.
The problem is that way too many are looking at masks as the Great White Hope. They aren’t. They make some slight difference, but are possibly doing more harm than good because people aren’t social distancing and washing because they think the masks are protecting them...
There’s a reason why this shit’s spiking in areas with mask mandates just as much as those that don’t... 85% of those testing positive are mask wearers....
@LuFins-Dad said in More masks....:
@jon-nyc said in More masks....:
This is really talking about being the guy with the mask in a community where mask usage is uncommon.
No, they specifically pointed out that mask usage in this community is unusually high.
The first sentence of George’s ‘long discussion’
n this community-based, randomized controlled trial conducted in a setting where mask wearing was uncommon
-
"... mask-wearing levels were reportedly high (88.7%) among people who did not catch the virus."
-
Hi - been a long time, since I've checked this forum.
I didn't read the entire article, but what is irritating is when employees of stores we shop at, as well as customers, wear a bandana, that they loosely just tie on, or a gaiter. Neither a bandana or gaiter help as well as a regular "single use" mask. I understand that grocery stores and other sites are pushing sales of gaiters, which people rarely wore in the past!
We are in the PURPLE here in California.@ILM said in More masks....:
Hi - been a long time, since I've checked this forum.
I didn't read the entire article, but what is irritating is when employees of stores we shop at, as well as customers, wear a bandana, that they loosely just tie on, or a gaiter. Neither a bandana or gaiter help as well as a regular "single use" mask. I understand that grocery stores and other sites are pushing sales of gaiters, which people rarely wore in the past!
We are in the PURPLE here in California.Don't be a stranger. Sometimes, we're interesting.
Except for Phibes, of course...
-
@LuFins-Dad said in More masks....:
@jon-nyc said in More masks....:
This is really talking about being the guy with the mask in a community where mask usage is uncommon.
No, they specifically pointed out that mask usage in this community is unusually high.
The first sentence of George’s ‘long discussion’
n this community-based, randomized controlled trial conducted in a setting where mask wearing was uncommon
@jon-nyc said in More masks....:
@LuFins-Dad said in More masks....:
@jon-nyc said in More masks....:
This is really talking about being the guy with the mask in a community where mask usage is uncommon.
No, they specifically pointed out that mask usage in this community is unusually high.
The first sentence of George’s ‘long discussion’
n this community-based, randomized controlled trial conducted in a setting where mask wearing was uncommon
I misread that the other way. My fault for skimming.
It still doesn’t change the general point of my post. Mask effectiveness is being blown way out of proportion. If mask wearing was that effective in controlling this crap, it would have been the first recommendation made by the CDC, not the last made months later...And even then slowly and with a bunch of caveats. In order of importance Social Distancing and hygiene are far more important. Unfortunately, everybody jumps on to the mask issue because it’s something visible and use it as a point of blame because we have to point the finger somewhere...
-
I can’t believe all those people at the Mayo Clinic didn’t wear masks... They ought to be ashamed! :eyeroll:
-
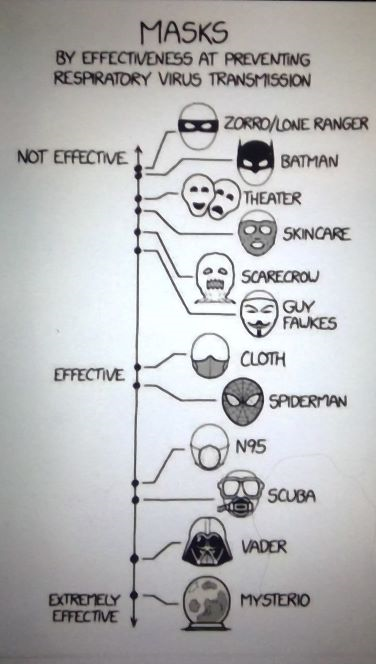
I've read that ordinary cloth 'hang round your ears' masks are maybe only maximkum 20% effective, while well-fitted N95/FPP2 worn correctly and tightly with elastic around the back of your head, actually covering nose and mouth so you breath through the material maybe up to 70% effective.
Considering both grandfathers endured eight hours a day six days a week in a dangerous, dirty job bent double mining coal, I think I can just about manage to stay indoors, keep my distance outside, and wear a mask.
-
@jon-nyc said in More masks....:
@LuFins-Dad said in More masks....:
@jon-nyc said in More masks....:
This is really talking about being the guy with the mask in a community where mask usage is uncommon.
No, they specifically pointed out that mask usage in this community is unusually high.
The first sentence of George’s ‘long discussion’
n this community-based, randomized controlled trial conducted in a setting where mask wearing was uncommon
I misread that the other way. My fault for skimming.
It still doesn’t change the general point of my post. Mask effectiveness is being blown way out of proportion. If mask wearing was that effective in controlling this crap, it would have been the first recommendation made by the CDC, not the last made months later...And even then slowly and with a bunch of caveats. In order of importance Social Distancing and hygiene are far more important. Unfortunately, everybody jumps on to the mask issue because it’s something visible and use it as a point of blame because we have to point the finger somewhere...
@LuFins-Dad I agree that mask wearing is just one part of an overall strategy. If none of the strategy parts are followed (or followed at less than 100% )the whole thing cannot work very well possibly.
Mask wearing
Good hygiene
social distancing
Detailed contact tracing
Quarantine -
Correlation Between Mask Compliance and COVID-19 Outcomes in Europe
Abstract
Masking was the single most common non-pharmaceutical intervention in the course of the coronavirus disease 2019 (COVID-19) pandemic. Most countries have implemented recommendations or mandates regarding the use of masks in public spaces. The aim of this short study was to analyse the correlation between mask usage against morbidity and mortality rates in the 2020-2021 winter in Europe. Data from 35 European countries on morbidity, mortality, and mask usage during a six-month period were analysed and crossed. Mask usage was more homogeneous in Eastern Europe than in Western European countries. Spearman's correlation coefficients between mask usage and COVID-19 outcomes were either null or positive, depending on the subgroup of countries and type of outcome (cases or deaths). Positive correlations were stronger in Western than in Eastern European countries. These findings indicate that countries with high levels of mask compliance did not perform better than those with low mask usage.....Conclusions
While no cause-effect conclusions could be inferred from this observational analysis, the lack of negative correlations between mask usage and COVID-19 cases and deaths suggest that the widespread use of masks at a time when an effective intervention was most needed, i.e., during the strong 2020-2021 autumn-winter peak, was not able to reduce COVID-19 transmission. Moreover, the moderate positive correlation between mask usage and deaths in Western Europe also suggests that the universal use of masks may have had harmful unintended consequences.Is "Cureus" a real publication? The (single) author is in Brazil.
-
It has an article on Ivermectin use too:
Conclusion: In this large PSM study, regular use of ivermectin as a prophylactic agent was associated with significantly reduced COVID-19 infection, hospitalization, and mortality rates.
-
I was Cureus
Cureus, also known as the Cureus Journal of Medical Science, is an open access general medical journal and is among the growing number of journals using prepublication and post publication peer review. It is also the first academic journal which provides authors with step-by-step templates for them to use to write their papers.[1] The journal's founders are John R. Adler (Stanford University), who serves as one of two editors-in-chief, and Alexander Muacevic (University of Munich) who serves as the second editor-in-chief.[2]
History and publication process
Cureus was originally started as PeerEMed in 2009, and was re-launched under its current name in December 2012.[1] Under its system, after an article is published, anyone can review it, but the reviews of experts will be given a higher score.[3] Its peer-review process involves asking experts to review a given article in a few days, which results in its peer reviews taking much less time than those of most other journals do.[3] Adler told Retraction Watch in 2015 that "Yes Cureus has an unusually fast review process, which is an important part of the journal’s philosophy. We believe that post publication peer review, a focus of our journal through commenting and our unique SIQ process, is potentially a more powerful way to discern truth."[4])