Half of med school graduates beginning surgical residency feel unprepared
-
A survey of 3693 first and second-year surgical residents found that 1775 (48.1%) said medical school did not adequately prepare them for the rigors of surgical residency.
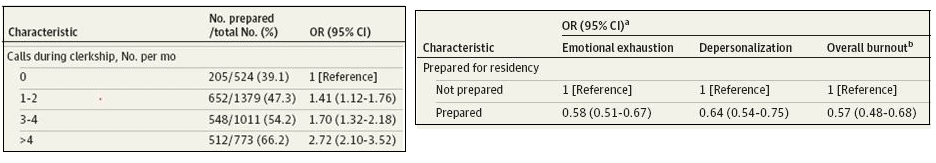
Taking overnight calls less than twice per month was reported by 51.6% during core surgery clerkships and 43.3% during subinternships. The more call students participated in, the more significantly likely they were to have felt adequately prepared for residency.
Of interest is that one third of those who took call more than 4 times per month still felt unprepared.
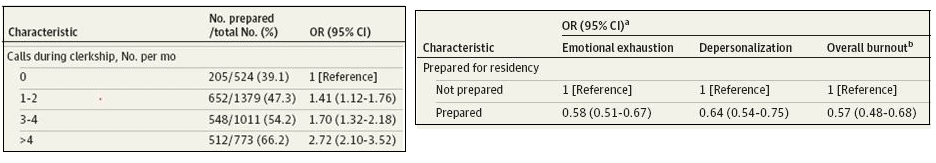
Residents who felt well prepared for surgical training reported significantly fewer symptoms of emotional exhaustion, depersonalization, and burnout.
The paper, published online in JAMA Surgery, surveyed residents who were training at hospitals that participated in the Flexibility in Duty Hour Requirements for Surgical Trainees (FIRST) trial. It was conducted at the time of an annual resident exam given by the American Board of Surgery, and the response rate was 99%.
Other factors limiting preparedness included rules and regulations limiting what students could do during clerkships and students acting as observers only when taking overnight call.
The investigators interviewed several faculty members and residents. One of the faculty noted that in the current culture, medical students were not allowed write progress notes. A female program director said, “I think that we’ve done a real disservice to the medical students at this point giving them an improper perception of what residency means and what going into surgery means in general.”
These findings did not surprise me. In 2010, one of my first blog posts was about this topic. I wrote, “The third-year surgery rotation in medical school is not a necessarily a good simulation of what it’s like to be a surgical resident.” The school I was with at the time had mandated that the students should be allowed to go to bed at 11 PM and they were only to be awakened for major cases.
I further explained this in a 2012 post on attrition in surgical residency programs saying, “I believe a major cause [of attrition] is that medical students do not understand what surgical residency training is really like. In some schools, third-year [surgical] clerkships are as short as 4 to 6 weeks, and part of that time may be spent on clinic or subspecialty rotations.” I also pointed out that many schools limited the amount of overnight call for students to once per week resulting in “an unrealistic picture of what a surgical residency is like.”
The authors of the JAMA Surgery paper concluded with this statement, “Adequate exposure to the necessary realities of surgical training and independent practice, particularly overnight call during the medical school clerkship, may [my emphasis] contribute to improved preparedness, lower attrition, and lower rates of burnout in general surgery residency.”
I hope the paper is widely read by medical and surgical educators.
=-=-=-=-=-=-=-=-=-=
4 calls per month? FOUR?
As a 3rd year med student I took between 8-12 calls per month.
-
A survey of 3693 first and second-year surgical residents found that 1775 (48.1%) said medical school did not adequately prepare them for the rigors of surgical residency.
Taking overnight calls less than twice per month was reported by 51.6% during core surgery clerkships and 43.3% during subinternships. The more call students participated in, the more significantly likely they were to have felt adequately prepared for residency.
Of interest is that one third of those who took call more than 4 times per month still felt unprepared.
Residents who felt well prepared for surgical training reported significantly fewer symptoms of emotional exhaustion, depersonalization, and burnout.
The paper, published online in JAMA Surgery, surveyed residents who were training at hospitals that participated in the Flexibility in Duty Hour Requirements for Surgical Trainees (FIRST) trial. It was conducted at the time of an annual resident exam given by the American Board of Surgery, and the response rate was 99%.
Other factors limiting preparedness included rules and regulations limiting what students could do during clerkships and students acting as observers only when taking overnight call.
The investigators interviewed several faculty members and residents. One of the faculty noted that in the current culture, medical students were not allowed write progress notes. A female program director said, “I think that we’ve done a real disservice to the medical students at this point giving them an improper perception of what residency means and what going into surgery means in general.”
These findings did not surprise me. In 2010, one of my first blog posts was about this topic. I wrote, “The third-year surgery rotation in medical school is not a necessarily a good simulation of what it’s like to be a surgical resident.” The school I was with at the time had mandated that the students should be allowed to go to bed at 11 PM and they were only to be awakened for major cases.
I further explained this in a 2012 post on attrition in surgical residency programs saying, “I believe a major cause [of attrition] is that medical students do not understand what surgical residency training is really like. In some schools, third-year [surgical] clerkships are as short as 4 to 6 weeks, and part of that time may be spent on clinic or subspecialty rotations.” I also pointed out that many schools limited the amount of overnight call for students to once per week resulting in “an unrealistic picture of what a surgical residency is like.”
The authors of the JAMA Surgery paper concluded with this statement, “Adequate exposure to the necessary realities of surgical training and independent practice, particularly overnight call during the medical school clerkship, may [my emphasis] contribute to improved preparedness, lower attrition, and lower rates of burnout in general surgery residency.”
I hope the paper is widely read by medical and surgical educators.
=-=-=-=-=-=-=-=-=-=
4 calls per month? FOUR?
As a 3rd year med student I took between 8-12 calls per month.
@George-K said in Half of med school graduates beginning surgical residency feel unprepared:
“Adequate exposure to the necessary realities of surgical training and independent practice, particularly overnight call during the medical school clerkship, may [my emphasis] contribute to improved preparedness,
Or, as a surgeon with whom I worked said, "The problem with being on call every other night is that you miss half the good cases."
-
Pussies
I took call every third night. Stayed in the whole next day. No Libby Zion laws.
Not that I think that it was sane , but surgery needs to be immersive. The only way to learn to be independent is to be there at two AM shitting your pants with worry and figuring out what to do.
Next generation of docs will be Computer savvy and up to date on all the new technologies , augemneted reality, hybrid ORs, robots. But I’m not sure what will be facing a knife in the chest, and no robot to help you open the chest in a few minutes.
-
Pussies
I took call every third night. Stayed in the whole next day. No Libby Zion laws.
Not that I think that it was sane , but surgery needs to be immersive. The only way to learn to be independent is to be there at two AM shitting your pants with worry and figuring out what to do.
Next generation of docs will be Computer savvy and up to date on all the new technologies , augemneted reality, hybrid ORs, robots. But I’m not sure what will be facing a knife in the chest, and no robot to help you open the chest in a few minutes.
@bachophile said in Half of med school graduates beginning surgical residency feel unprepared:
Libby Zion laws.
Is there any evidence that those laws made a difference in outcomes, or reduced mistakes?
-
The only help they may have done was reduced car accidents of residents driving home after call.
-
Which is something...
-
When I told Mrs. George about this article, she reminded me...
"Remember when you were a resident on OB, and because of a lack of staff, you were on call every other night?"
Oh...yeah.
That was a lifetime ago, of course, and the residency was quite different (not as busy - I could usually get 2-3 hours of uninterrupted sleep).
Is more frequent call a good thing, ultimately?
I don't know.
This report seems to suggest that entering a residency while not having a rich late-night experience is detrimental, at least in terms of "feeling prepared."
My experience was remarkable. The day after I grabbed my diploma, I was 100% ready, with no anxiety. I was confident in what I knew, and I was confident that I would have support from my senior colleagues (my resident) that he would help me if I needed it.
It was not a surgical residency, but a medical one, but I think the basic point stands - my schooling made me ready.