Today's MedMal case - snakebite
-
A 13-year-old girl was bitten on her foot by a rattlesnake at around 8:20pm.
Her father killed it, took a picture, and called 911.
They brought the dead snake to the ED as well.
The patient was seen by the ER doctor at 9:20pm.
This is how her foot looked shortly after arrival to the ED:

The doctor and nurses initiated the hospital’s snakebite protocol.
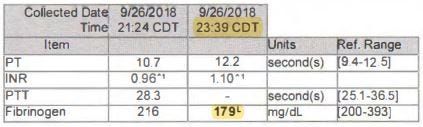
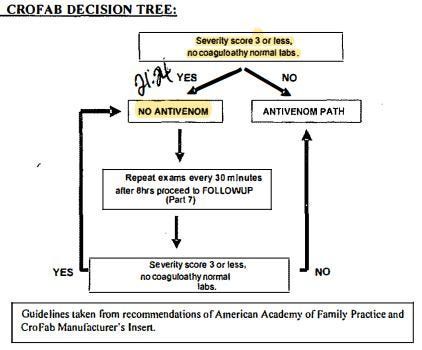
They filled out a Snakebite Severity Score (SSS).
She was initially given a 2, then revised upward to a 3 several minutes later due to development of paresthesias (numbness and tingling) in the toes.
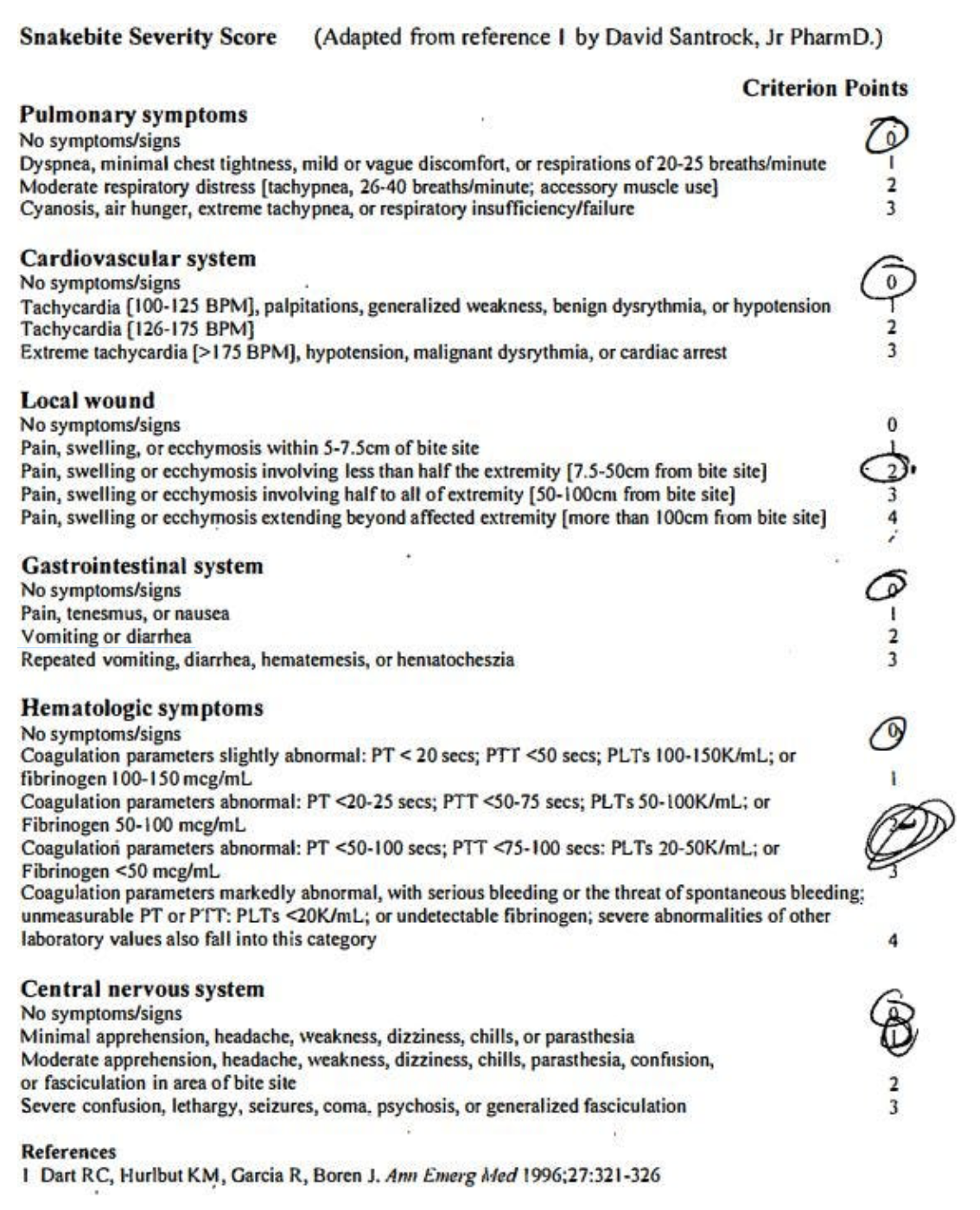
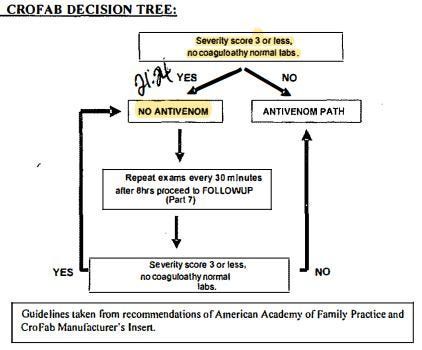
They decided not to give Crofab based on the protocol’s decision tree.
The patient’s pain began to creep up her leg.
The areas of pain were marked at different times during the nurse’s reassessments.

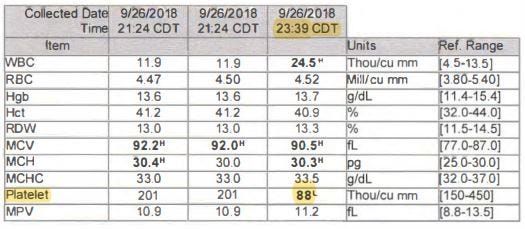
Repeat labs were drawn at 23:39, showing decreased fibrinogen and thrombocytopenia.
Her Snakebite Severity Score had risen to a 5.
The doctor ordered Crofab at 23:50 and the infusion was done by 00:29.
The patient was transferred to a pediatric medical center
At the receiving hospital, the redness and swelling significantly worsened.
She was given additional Crofab.
After several days, the appearance of her leg was improving.
She worked with physical therapy and was discharged with crutches.
The patient and her family report permanent pain and dysfunction in her leg.
The patient’s family was very upset about her lingering symptoms.
They blamed the doctor for not giving Crofab immediately upon arrival.
The hospital agreed to write off the entire bill (Crofab alone was $69,788.25).
The state in which this happened has a law that requires plaintiffs to demonstrate that the defendants acted with “willful and wanton” negligence if the case involves emergency care.
The judge felt the doctor’s actions did not rise to this level, and dismissed the lawsuit.
The plaintiffs appealed.
They argued that only a physician can practice medicine, not a hospital protocol.
In their eyes, the doctor displayed gross negligence by not immediately giving Crofab, even if the hospital protocol said otherwise.
The appeals court reversed the initial judge’s decision.
The defense then appealed to the state’s Supreme Court.
The Supreme Court reversed the appeals courts’ decision and reinstated the trial court’s dismissal of the lawsuit.
-
Reviewer Analysis:
-
I agree with the Supreme Court that the doctor did not display willful or wanton negligence. Crofab is not a risk-free medication, and it is extremely unwise to advocate instantly ordering it for any relevant envenomation. The package insert for Crofab notes hypotension and angioedema as possible risks. The thoughtful approach the doctor displayed by following the algorithm is the correct way to balance the risks and benefits involved with both the snakebite itself and the administration of Crofab.
-
I find the expert’s opinion somewhat disturbing at several points.
a) It is littered with state-specific legal buzzwords that make it clear that it was heavily coached by the plaintiff’s attorney. A physician’s opinion should stick to the medical facts and experts should not allow attorneys to inject their own parasitic language that perverts the doctor’s sober analysis.
b) He acts as if the unified treatment algorithm for the management of crotaline snakebite in the US is the absolute and definitive treatment algorithm. In fact, the studies that the Crofab manufacturer cite used the Snakebite Severity Score to guide administration (not the unified treatment algorithm). His claims do not accurately reflect the ambiguity involved when different algorithms provide different recommendations for the exact same clinical scenario.
c) The expert states that he called and spoke with the patient’s mother. This is very bizarre. I’ve reviewed thousands of lawsuits, and I’ve never seen an expert mention that they personally called a patient or family member. An expert might review a deposition of a family member, or an independent medical exam (IME) might be conducted by a doctor, but most experts don’t call the plaintiffs and conduct their own homemade deposition. This is an obvious source of bias, especially in light of the fact that he never called the defending doctor to get her side of the story.
- ACEP’s lawyers filed an amicus curiae brief with the Supreme Court on behalf of the doctor. This was an important piece of advocacy given that this case threatened to erode the “willful and wanton” / gross negligence standard in this state. Many EM physicians have mixed feelings about ACEP, but I would be remiss to not point out the importance of their advocacy for this individual physician and the specialty as a whole.
-
-
A 13-year-old girl was bitten on her foot by a rattlesnake at around 8:20pm.
Her father killed it, took a picture, and called 911.
They brought the dead snake to the ED as well.
The patient was seen by the ER doctor at 9:20pm.
This is how her foot looked shortly after arrival to the ED:

The doctor and nurses initiated the hospital’s snakebite protocol.
They filled out a Snakebite Severity Score (SSS).
She was initially given a 2, then revised upward to a 3 several minutes later due to development of paresthesias (numbness and tingling) in the toes.
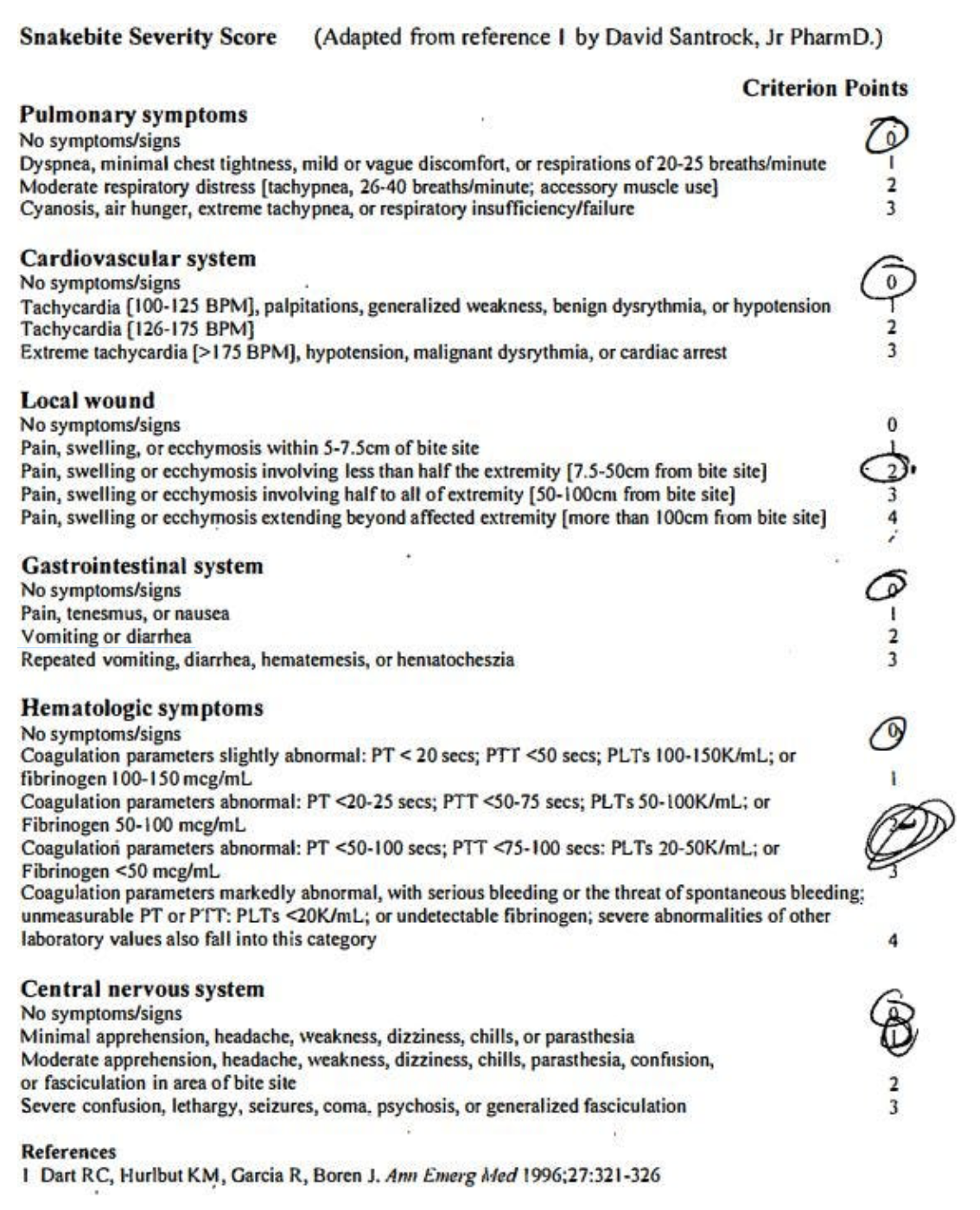
They decided not to give Crofab based on the protocol’s decision tree.
The patient’s pain began to creep up her leg.
The areas of pain were marked at different times during the nurse’s reassessments.

Repeat labs were drawn at 23:39, showing decreased fibrinogen and thrombocytopenia.
Her Snakebite Severity Score had risen to a 5.
The doctor ordered Crofab at 23:50 and the infusion was done by 00:29.
The patient was transferred to a pediatric medical center
At the receiving hospital, the redness and swelling significantly worsened.
She was given additional Crofab.
After several days, the appearance of her leg was improving.
She worked with physical therapy and was discharged with crutches.
The patient and her family report permanent pain and dysfunction in her leg.
The patient’s family was very upset about her lingering symptoms.
They blamed the doctor for not giving Crofab immediately upon arrival.
The hospital agreed to write off the entire bill (Crofab alone was $69,788.25).
The state in which this happened has a law that requires plaintiffs to demonstrate that the defendants acted with “willful and wanton” negligence if the case involves emergency care.
The judge felt the doctor’s actions did not rise to this level, and dismissed the lawsuit.
The plaintiffs appealed.
They argued that only a physician can practice medicine, not a hospital protocol.
In their eyes, the doctor displayed gross negligence by not immediately giving Crofab, even if the hospital protocol said otherwise.
The appeals court reversed the initial judge’s decision.
The defense then appealed to the state’s Supreme Court.
The Supreme Court reversed the appeals courts’ decision and reinstated the trial court’s dismissal of the lawsuit.
-
I'm lousy at coag beyond the basics. It's definitely an intrinsic pathway problem...Taking a SWAG, maybe factor 9 or 10 is screwed up, and fibrinogen is being sucked up in some type of thrombosis formation?
And ...That could be an actual screw-up of an answer...
-
I'm lousy at coag beyond the basics. It's definitely an intrinsic pathway problem...Taking a SWAG, maybe factor 9 or 10 is screwed up, and fibrinogen is being sucked up in some type of thrombosis formation?
And ...That could be an actual screw-up of an answer...
@Jolly here is a recent article on fibrinogen in snake bites if you r interested.
https://www.mdpi.com/2072-6651/14/8/538
All gobbledigook to me. Just say DIC and call it a day.
-
Vipers kill. As
pk cleopatra -
I didn't know that rattlesnake bites can be that bad! Wow.
It seems to be bizarre to sue the doctor when he followed the guidelines he was given.
@Klaus said in Today's MedMal case - snakebite:
It seems to be bizarre to sue the doctor when he followed the guidelines he was given.
One thing that was drummed into our heads, especially in private practice, was to "Follow the protocol."
If there's ever a bad event, the first thing the plaintiif's attorney will ask is, "Doctor, is there a protocol in your hospital for this event?"
If there is, and you didn't follow it, you're screwed.
If there isn't, you rely on your judgment.
@bachophile said in Today's MedMal case - snakebite:
All gobbledigook to me.
Coagulation and renal physiology were my two weakest areas of knowledge.
-
I am not a doctor (and never play on on TV), but it seemed like the doctor in this case did do the best treatment based on diagnosis.
-
Update:
I wanted to share 2 pieces of additional information related to the recent Snake Bite case.
The most important is the feedback that I got from several toxicologists.
They advised that using the Snakebite Severity Score (SSS) to guide the decision to give Crofab was not ideal.
The SSS was developed for research purposes, not to guide clinical care.
In fact, the lead author of the SSS (Dr. Richard Dart) wrote a letter in 1996 saying that it was not meant to guide treatment of individual patients, and that further research should be done to validate it for clinical use.
Most of the toxicologists I got feedback from suggested that they would give Crofab immediately for any rattlesnake bite that shows any sign of true envenomation.
Agkistrodon species (water mocassins, cotton mouth) bites are often less severe than rattlesnake bites, and it seems that some experts might be more inclined to use an algorithm (Unified treatment algorithm, not SSS) to guide decision-making, although there is debate about this.
The toxicologists also point out that the doctor could have called poison control to get expert advice, as opposed to relying on the questionable hospital protocol that led to delayed Crofab administration.
I still don’t think the doctor displayed gross negligence or “willful and wanton” negligence.
The court got it right when they threw the case out.
If anything, the hospital itself should be criticized for giving their doctors substandard policies.
There is wide geographic variation in how much residents are taught about managing snake bites, which means that many doctors with limited snakebite experience (including myself) may rely more heavily on hospital policies that might actually be poorly informed.
-
Was the father exhibiting common sense, in taking a picture of the snake and having it picked up?
Isn't the size of the snake of some significance in determining whether to give the anti-venom?
Why won't they mention which state this occurred in, and city, if it did take place in a city. What is the protocol for the paramedics when there is clear evidence of venomous snake bite, and consideration of the length of time to the hospital?