Today's medical mysterie.
-
The ER doc hasn't posted the answer (it'll be there tomorrow).
@blondie got it.
Compare the right and left sides of the picture. There are no lung markings on the (patient's) left. Heart is pushed to the (patient's) right.
Impressive that vital signs are stable.
-
Around 1987 (!) I was sitting in our small office in the OR at the university. I was at the desk, running the schedule. One of my colleagues. to my left suddenly said, "I can't breathe!" He looked like shit.
We took him to pre-op holding where a portable chest x-ray confirmed a spontaneous right pneumothorax. There was a (not very good) chest surgeon in the hospital in the hospital at the time and a right-sided chest tube was inserted in pre-op holding. He spent about 4 days in the hospital and was discharged with no sequelae.
He said that inserting the chest tube was the most painful thing imaginable.
-
-
A bit obvious . The danger is tension pneumothorax where the increasing pressure on the affected side presses on the IVC diminishing venous return to the heart and ultimately having cardiac output drop to…..
Easy fix is jamming a small needle in the second intercostal space and hearing the ppppfffssssstt leak out, turning it into an open pneumothorax, then u can wait for someone with a more “delicate” hand to put into the tube. I’ve put in countless tubes in trauma situations. In my younger years when when I considered trauma vaguely interesting. Now I detest trauma and avoid it like the plague. Just a big pain in the butt.
For the younguns who like Adrenalin rushes. I’m over the hill. Seen that done that. -
OK, here's XRayGPT's take.
Upon reviewing this chest X-ray, here are the key observations:
1. Lung Fields: Both lungs appear well-aerated with no focal consolidation, pleural effusion, or pneumothorax visible. The lung markings are symmetrical and extend to the periphery without any obvious abnormal opacities. 2. Cardiomediastinal Contour: The heart size is within normal limits, and there is no visible widening of the mediastinum. The aortic arch appears normal, with no signs of enlargement. 3. Bony Structures: The ribs, clavicles, and visible parts of the spine do not show any fractures or lytic lesions. The bones appear intact. 4. Diaphragm and Costophrenic Angles: The diaphragms are well-defined, with sharp costophrenic angles bilaterally. No subdiaphragmatic free air is observed, which would suggest pneumoperitoneum.Impression
This is a normal chest X-ray with no evident pathology. If the patient is symptomatic, further investigation might be necessary, as subtle or early pathologies (e.g., small nodules or early interstitial lung disease) may not be readily visible on standard X-ray.
If there’s any relevant history or clinical symptoms, feel free to share them, as they could guide additional diagnostic steps.*
Then I asked it to look at the left side.
Thank you for directing my attention. Upon closer examination of the left side of the chest X-ray, the following observation stands out:
• There is a relative increase in radiolucency (darkness) on the left side, particularly in the upper and mid-lung zones. This increased radiolucency suggests a potential left-sided pneumothorax or hyperinflation of the left lung. • The lung markings appear to be diminished or absent in the outer portion of the left hemithorax, which further supports the suspicion of a pneumothorax. • Additionally, the left hemidiaphragm and left lateral costophrenic angle are visible, without any obscuring opacities, which is consistent with a pneumothorax rather than effusion.Impression
This X-ray is suggestive of a left-sided pneumothorax. The absence of lung markings in the periphery and the increased radiolucency on the left side are key indicators. However, confirming the size and clinical significance of this pneumothorax would be essential, as well as assessing the patient’s respiratory status to determine if urgent intervention is needed.
If the patient has symptoms like sudden shortness of breath, chest pain, or hypoxia, they may require immediate treatment.*
I wonder how well a specialized AI model would do in such cases. My guess is that it's way better.
-
OK, here's XRayGPT's take.
Upon reviewing this chest X-ray, here are the key observations:
1. Lung Fields: Both lungs appear well-aerated with no focal consolidation, pleural effusion, or pneumothorax visible. The lung markings are symmetrical and extend to the periphery without any obvious abnormal opacities. 2. Cardiomediastinal Contour: The heart size is within normal limits, and there is no visible widening of the mediastinum. The aortic arch appears normal, with no signs of enlargement. 3. Bony Structures: The ribs, clavicles, and visible parts of the spine do not show any fractures or lytic lesions. The bones appear intact. 4. Diaphragm and Costophrenic Angles: The diaphragms are well-defined, with sharp costophrenic angles bilaterally. No subdiaphragmatic free air is observed, which would suggest pneumoperitoneum.Impression
This is a normal chest X-ray with no evident pathology. If the patient is symptomatic, further investigation might be necessary, as subtle or early pathologies (e.g., small nodules or early interstitial lung disease) may not be readily visible on standard X-ray.
If there’s any relevant history or clinical symptoms, feel free to share them, as they could guide additional diagnostic steps.*
Then I asked it to look at the left side.
Thank you for directing my attention. Upon closer examination of the left side of the chest X-ray, the following observation stands out:
• There is a relative increase in radiolucency (darkness) on the left side, particularly in the upper and mid-lung zones. This increased radiolucency suggests a potential left-sided pneumothorax or hyperinflation of the left lung. • The lung markings appear to be diminished or absent in the outer portion of the left hemithorax, which further supports the suspicion of a pneumothorax. • Additionally, the left hemidiaphragm and left lateral costophrenic angle are visible, without any obscuring opacities, which is consistent with a pneumothorax rather than effusion.Impression
This X-ray is suggestive of a left-sided pneumothorax. The absence of lung markings in the periphery and the increased radiolucency on the left side are key indicators. However, confirming the size and clinical significance of this pneumothorax would be essential, as well as assessing the patient’s respiratory status to determine if urgent intervention is needed.
If the patient has symptoms like sudden shortness of breath, chest pain, or hypoxia, they may require immediate treatment.*
I wonder how well a specialized AI model would do in such cases. My guess is that it's way better.
@Klaus said in Today's medical mysterie.:
I wonder how well a specialized AI model would do in such cases. My guess is that it's way better.
I've read that AI-assisted radiology is remarkably good, particularly for breast imaging. @bachophile knows more about that than I do.
-
And here I thought he problem was that he was see through. I mean, you can see past his skin and blood and everything. That’s nuts!
-
every one of our chest X-rays in my institution (must be hundreds a day) undergo AI reading in addition to being read by a radiologist. This has resulted in numerous call backs for CTs because of missed small lesions susp for lung cancer.
Yes in breast imaging also pretty sharp but we don’t have that incorporated automatically like chest films.
We also are beginning to use AI in pathology slide readings. -
every one of our chest X-rays in my institution (must be hundreds a day) undergo AI reading in addition to being read by a radiologist. This has resulted in numerous call backs for CTs because of missed small lesions susp for lung cancer.
Yes in breast imaging also pretty sharp but we don’t have that incorporated automatically like chest films.
We also are beginning to use AI in pathology slide readings.@bachophile said in Today's medical mysterie.:
We also are beginning to use AI in pathology slide readings.
Makes sense. Head scratchers do occur.
-
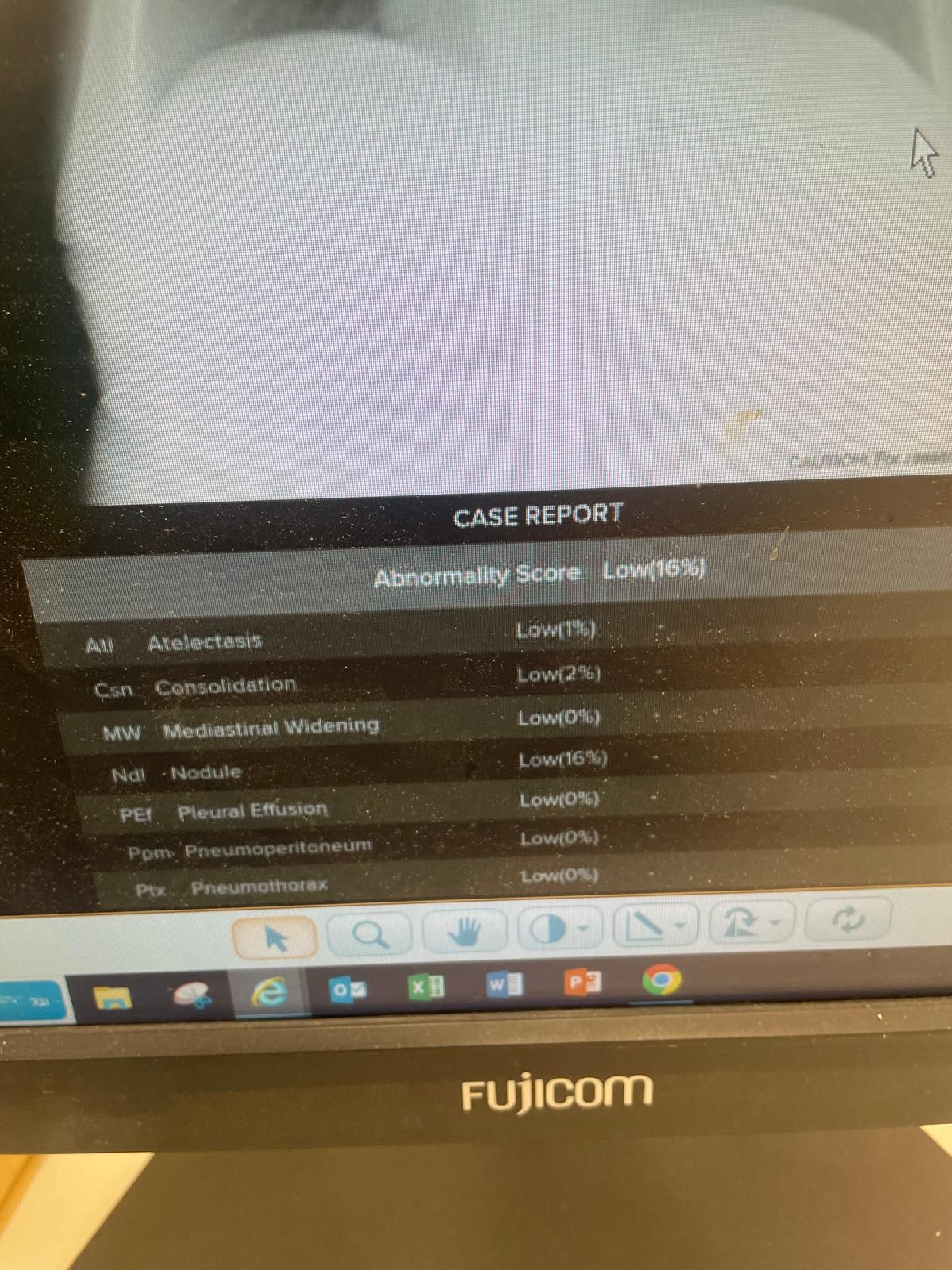
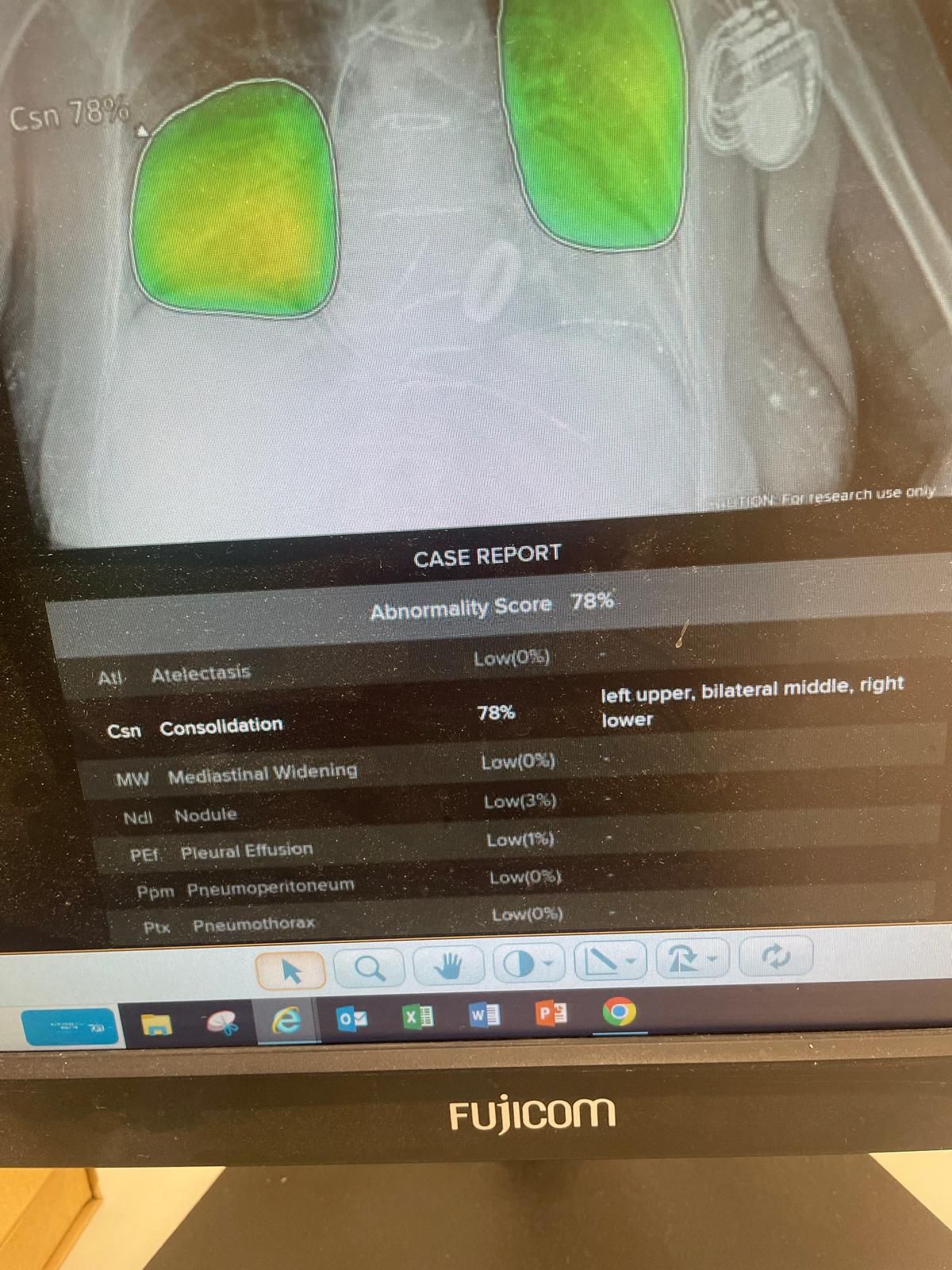
Just an example of two random chest X-rays I pulled up just now. On the bottom of each is the abnormality score rated by an AI. One was completely normal. The other showed a bilateral pneumonia. Those would be seen easily anyway. The tricky ones are the small nodules which can be missed and may be early lung cancer. And it works. We have picked up otherwise occult cancers missed by the radiologist.


