LFV in the OR
-
-
We did that for a while, just because it made sense. Didn't have the science.
From the paper:
Once patients were on CPB, the ventilation was set up at a respiratory rate of 5 inflations/min with air (21% oxygen) at a tidal volume of 6 to 8 mL/kg and PEEP of 5 cmH2O according to a standardized protocol.
I can see surgeons complaining about the lung getting into their field of view every 12 seconds. Also PEEP (positive end-expiratory pressure) of 5 cmH2O is not a lot, but it might be enough to compromise visibility as well.
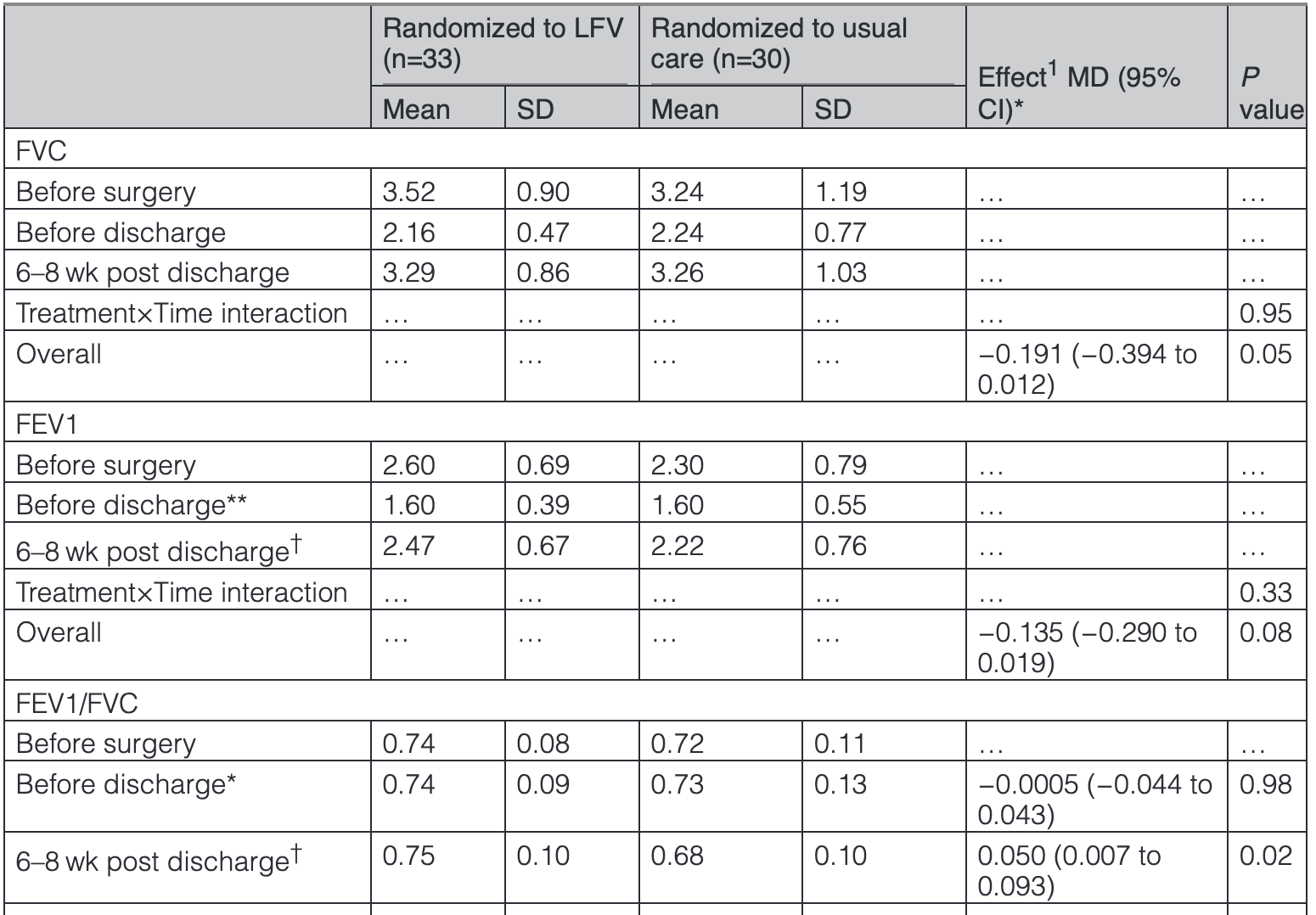
The differences in vital capacity between the groups after negligible. Airflow (FEV1/FVC) seems to show a bigger difference (68% vs 75%).
Though statistically significant, the question is always "Is it clinically significant?"
Postoperative clinical complications are reported only descriptively as the trial was not powered for these measures. These occurred overall in 9/63 patients, of whom 5/33 were in the LFV group and 4/30 in the UC group (relative risk, 1.24 [95% CI, 0.39–3.91]). Lung complications, time fit for discharge, and adverse events postsurgery up to 6 to 8 weeks post discharge are reported in Tables S5 through S7. There were no postoperative deaths, myocardial infarctions, permanent strokes, or cases of renal failure requiring dialysis. No differences were observed for serious adverse events, intensive care length of stay, or hospital length of stay.