Elective Surgery and Ozempic
-
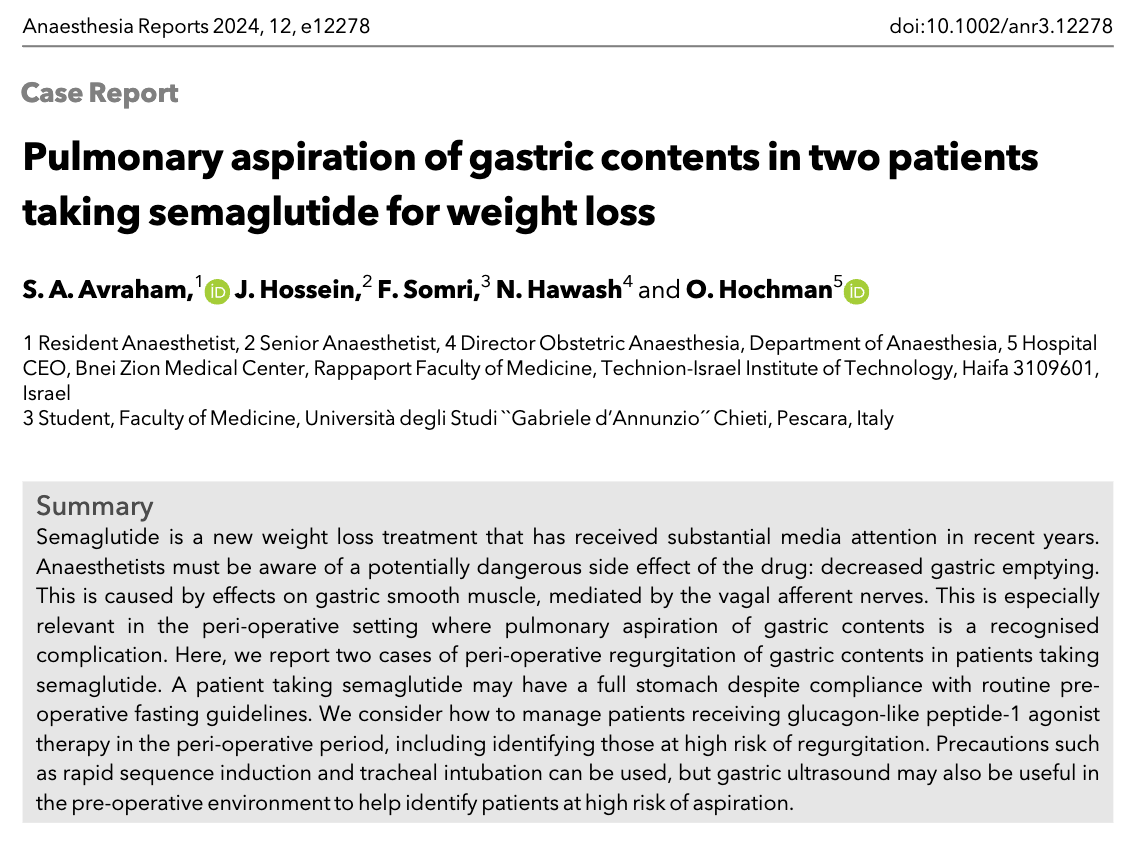
One of the mechanisms by which GLP-1 agonists (like Ozempic, Wygovy, etc) cause weight loss is by delaying gastric emptying. So, your stomach doesn't empty and you feel "full" longer. Of course, there are side effects to this, and, I've read that, at higher doses, up to 40% of patients taking these drugs experience nausea and vomiting.
Of course, a "full stomach" is a major concern for any anesthesiologist. I've seen one patient die from aspiration of gastric contents (not my case, btw).
So, the American Society of Anesthesiologists has come up with guidelines for taking care of patients on GLP-1 agonists:
Day or week prior to the procedure:
- Hold GLP-1 agonists on the day of the procedure/surgery for patients who take the medication daily.
- Hold GLP-1 agonists a week prior to the procedure/surgery for patients who take the medication weekly.
- Consider consulting with an endocrinologist for guidance in patients who are taking GLP-1 agonists for diabetes management to help control their condition and prevent hyperglycemia (high blood sugar).
Day of the procedure:
- Consider delaying the procedure if the patient is experiencing GI symptoms such as severe nausea/vomiting/retching, abdominal bloating or abdominal pain and discuss the concerns of potential risk of regurgitation and aspiration with the proceduralist or surgeon and the patient.
- Continue with the procedure if the patient has no GI symptoms and the GLP-1 agonist medications have been held as advised.
- If the patient has no GI symptoms, but the GLP-1 agonist medications were not held, use precautions based on the assumption the patient has a “full stomach” or consider using ultrasound to evaluate the stomach contents. If the stomach is empty, proceed as usual. If the stomach is full or if the gastric ultrasound is inconclusive or not possible, consider delaying the procedure or proceed using full stomach precautions. Discuss the potential risk of regurgitation and aspiration of gastric contents with the proceduralist or surgeon and the patient.
Full stomach precautions also should be used in patients who need urgent or emergency surgery.
I can see it becoming standard that getting an ultrasound of the stomach before surgery becomes almost commonplace to ensure an empty stomach.
-
Lawsuit Alleges Untold Stomach Risks
A new lawsuit from a woman with type 2 diabetes alleges that the makers of the drugs Ozempic and Mounjaro did not provide adequate warnings for the severity of stomach problems caused by the popular medicines.
The two drugs, which are FDA-approved to treat type 2 diabetes, have become well known for their weight loss properties. Ozempic is made by Danish drugmaker Novo Nordisk, and Mounjaro is made by Indiana-based Eli Lilly and Co.
In the lawsuit, Jaclyn Bjorklund, 44, of Louisiana, asserts that she was “severely injured" after using Ozempic and Mounjaro and that the pharmaceutical companies failed to disclose the drugs' risk of causing vomiting and diarrhea due to inflammation of the stomach lining, as well as the risk of stomach paralysis. (The medical term for stomach paralysis is gastroparesis.)
The prescribing labels for Mounjaro and Ozempic state that each “delays gastric emptying" and warn of the risk of severe gastrointestinal adverse reactions. The prescribing labels for both drugs state that the most common side effects include vomiting, diarrhea, and stomach pain. The Ozempic label does not mention gastroparesis, and the Mounjaro label states that the drug has not been studied in people with the condition and is therefore not recommended for people who have it.
Bjorklund has not been diagnosed with gastroparesis, but her symptoms are “indicative of" the condition, her lawyer, Paul Pennock, told NBC News.
Bjorklund used Ozempic for more than one year, and in July 2023 switched to Mounjaro, the lawsuit states. The document, posted on her law firm's website, details that using the drugs resulted in “severe vomiting, stomach pain, gastrointestinal burning, being hospitalized for stomach issues on several occasions including visits to the emergency room, [and] teeth falling out due to excessive vomiting, requiring additional medications to alleviate her excessive vomiting, and throwing up whole food hours after eating."
I don't get it.
-
The side effects are documented in the prescribing information. The prescribing doc should have alerted her to the possibility.
-
The drug lasts about a week (hence the need for weekly injections). If she was having such severe side effects, why did she continue?
-
She "switched" from Ozempic to Mounjaro. The drugs have similar mechanisms of action. I'm not surprised that the problem persisted.
-
The story says that the labels don't mention "gastroparesis." That's what "delayed gastric emptying" is.
-
-
Another warning about Ozempic (and other GLP-1 agonists).
The FDA added the postmarketing reports of ileus, or blocked intestines, to the drug labelingopens in a new tab or window for semaglutide (Ozempic).
"Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure," the drug label notes.
The injectable GLP-1 receptor agonist is indicated for type 2 diabetes, but its popularity as an off-label weight-loss drug has skyrocketed.
Labeling for semaglutide 2.4 mg (Wegovy) -- indicated for obesity -- already reflects the potential adverse reactionopens in a new tab or window based on postmarketing reports, noting that gastrointestinal disorders can include "acute pancreatitis and necrotizing pancreatitis, sometimes resulting in death, ileus."
Ileus can cause cramping and pain, the inability to have a bowel movement, swelling, vomiting, or lack of appetite, according to the Mayo Clinic. It often leads to hospitalizationopens in a new tab or window to first stabilize the condition, followed by a barium or air enema or, for complete intestinal obstruction, surgery. For a pseudo-obstruction, a doctor may prescribe medication to cause muscle contractions, stop the medication causing the obstruction, or use a decompression treatment.
Labeling for tirzepatide (Mounjaro), a dual GIP/GLP-1 receptor agonist approved for type 2 diabetes, was changed to addopens in a new tab or window ileus as a potential side effect based on postmarketing reports in July.
Both drugs can also cause gastroparesis, a delay of the stomach emptying process in which normal contraction of the stomach muscles is slowed down or even stopped, which has become a safety concern of late for surgical patientsopens in a new tab or window due to the risk of aspiration. Drug labels for both mention "delay of gastric emptying" under potential drug interactions, but not under warnings or adverse events.
One of my former colleagues died of necrotizing pancreatitis. Not a pleasant way to go.
-
What is a "pt" and what is induction?
-
What is a "pt" and what is induction?
@taiwan_girl said in Elective Surgery and Ozempic:
What is a "pt"
"Patient."
and what is induction?
Induction of anesthesia -
starting a drug-induced comaputting someone to "sleep. -
Aspiration of gastric contents is a very bad thing. It is the anesthesiologist's nightmare. Well, one of several, actually.
I've had it happen to me once - a pediatric case who had been NPO for at least 12 hours. He recovered fine.
One of my partners had a lady with a hiatal hernia. As soon as he put her to sleep, everything came up into her mouth...and down her trachea. She died in the ICU about a week later.